
Infertility is commonly defined as the inability to get pregnant after one year of regular unprotected sex, leading to difficulties in conception. Couples with women over 35 years old often begin the diagnostic evaluation after six months of unsuccessful attempts to conceive, seeking solutions for spontaneous pregnancy. The American Society for Reproductive Medicine (ASRM) has established guidelines for assessing infertility, which includes analyzing semen and sperm quality, checking ovulation, conducting a hysterosalpingogram, and, if necessary, performing tests for ovarian reserve and laparoscopy. When all these tests come back normal, doctors diagnose the couple with unexplained infertility, despite the use of clomid or other fertility treatments. Although the exact likelihood may vary, it means that all the test results show no apparent cause for the couple’s infertility.
Assessment of Male Infertility
Around 30% of couples experience male factor infertility as the sole cause, while it contributes to another 20% to 30% of cases. When assessing infertility in couples, it is important to evaluate the male partner through a comprehensive process involving their medical history, physical examination, and semen analysis. Key factors in the medical history include previous instances of fatherhood, a history of cryptorchidism, past medical and surgical procedures, sexual dysfunction, and any use of medications, tobacco, alcohol, or illegal drugs. Additionally, assessing sperm quality is crucial to understanding the causes of male factor infertility. During the physical examination, abnormalities such as varicoceles or the absence of the vas deferens can be identified. In some cases, clomid or IVF treatment may be recommended.
If the semen analysis shows abnormalities, it is recommended to repeat the test after at least one month at a laboratory that follows the World Health Organization (WHO) guidelines for unexplained infertility diagnosis. The laboratory should have a quality control program in place to ensure accurate testing for idiopathic infertility. The WHO has published guidelines that provide reference ranges for the number, morphology, and motility of sperm in a semen sample for infertility cases. However, different commercial laboratories may use their own ranges for these components in the context of infertility treatment. It is important to pay close attention to these ranges and interpret the semen values in the appropriate context for diagnosing unexplained infertility. While semen analysis is commonly used to assess the male partner in infertile couples, the specific ranges for determining fertility levels are not clearly defined for idiopathic infertility. A study conducted by Guzick and colleagues concluded that certain threshold values for sperm concentration, motility, and morphology can be used to classify men as subfertile or of indeterminate fertility status in cases of unexplained infertility diagnosis.
Table 1
World Health Organization Criteria for a Normal Semen Analysis
| Criteria | Parameters |
|---|---|
| Volume | 2.0–5.0 mL |
| pH | 7.2–7.8 |
| Sperm concentration | ≥ 20 × 106/mL |
| Total sperm count | ≥ 40 × 106 spermatozoa |
| Motility | ≥ 50% with forward progression or ≥ 25% with rapid |
| linear progression within 60 min after collection | |
| Morphology | ≥ 50% with normal morphology |
| Viability | ≥ 75% live (ie, excluding dye) |
| White blood cells | ≤ 1 × 106/mL |
| Fructose (total) | ≥ 13 mol/ejaculate |
Table 2
Fertile, Indeterminate, and Subfertile Ranges for Semen Analysis Parameters as Identified by Regression Analysis
| Semen Measurement | |||
|---|---|---|---|
| Concentration | Motility | Morphology | |
| Variable | (× 106/mL) | (%) | (% Normal) |
| Fertile range | > 48.0 | > 63 | > 12 |
| Indeterminate range | 13.5–48.0 | 32–63 | 9–12 |
| Univariate odds ratio | 1.5 (1.2–1.8) | 1.7 (1.5–2.2) | 1.8 (1.4–2.4) |
| for infertility (95% CI) | |||
| Subfertile range | < 13.5 | < 32 | < 9 |
| Univariate odds ratio | 5.3 (3.3–8.3) | 5.6 (3.5–8.3) | 3.8 (3.0–5.0) |
| for infertility (95% CI) |
n the past, the postcoital test (PCT) was commonly used to assess sperm motility in the cervical mucus after intercourse as part of the basic infertility evaluation for infertile couples. However, previous studies have shown that there is not a strong connection between postcoital sperm motility and the likelihood of getting pregnant for infertile couples. Additionally, a blinded study conducted in 1995 found that trained observers had difficulty reproducing consistent results with the test, which raises doubts about its reliability as a diagnostic tool for diagnosing infertility problems. As a result, the PCT is no longer widely used and we do not recommend including it in the standard investigation of infertility diagnosis for infertile couples.
Assessment of Ovulation
Ovulatory defects are present in 40% of infertile women and in approximately 15% of couples with infertility. Often a defect in ovulatory function manifests itself in menstrual disturbances and can be identified by history in the majority of women. Providers should investigate a patient with menstrual abnormalities for underlying causes such as polycystic ovarian syndrome, thyroid disease, hyperprolactinemia, and hypothalamic causes secondary to weight changes. Eumenorrhea—normal menstrual cycles by history—is a highly accurate marker of ovulation and anovulatory levels of serum progesterone (< 3 ng/mL) are found in only a very small minority of eumenorrheic patients. Support from healthcare professionals is crucial in addressing these issues. Additionally, assisted reproductive technology (ART) may be considered for couples experiencing infertility.
To assess ovulation and fertility, various methods are employed, including recording basal body temperature (BBT), using urinary luteinizing hormone (LH) ovulation predictor kits, conducting mid luteal serum progesterone tests, and performing endometrial biopsies to evaluate secretory endometrial development. BBT recordings, although the most cost-effective option, can be challenging to interpret and often cause frustration for patients. Ovulation predictor kits are beneficial for women with shorter menstrual cycles and help couples time intercourse appropriately. Mid luteal progesterone levels are typically measured on day 21 for women with regular (∼ 28 day) cycles, but this timing may not be accurate for those with irregular periods. In such cases, it is better to use an ovulation kit and measure progesterone levels 7 to 8 days later. These fertility testing methods can provide valuable support to patients and their providers.
This chart displays an example of recording basal body temperature to support fertility tracking. It has been taken from Hyde and DeLamater’s book, Understanding Human Sexuality, 6th edition. The copyright for this chart belongs to The McGraw-Hill Companies, Inc. Fertility providers may use this chart to determine the cause of infertility.
Assessment of Ovarian Reserve
IInfertility in couples can be further examined by assessing ovarian reserve. Women who are older or have had previous ovarian surgery are more likely to have diminished ovarian function or reserve. Many healthcare professionals now consider evaluating ovarian reserve as the initial step in diagnosing infertility due to its relatively noninvasive nature. This evaluation typically involves measuring follicle-stimulating hormone (FSH) and estradiol levels on cycle day 3, conducting a clomiphene citrate challenge test, and/or performing an ultrasonographic ovarian antral follicle count. While these tests do not provide definitive evidence of infertility, abnormal results are often associated with reduced response to ovulation induction medications and lower success rates in achieving live births through in vitro fertilization (IVF). These assessments support healthcare providers in determining appropriate treatment options for couples facing infertility.
Assessment of Uterus and Fallopian Tubes
Assessing the shape of the uterus and the openness of the fallopian tubes is an important part of the basic evaluation for infertility. One way to do this is through a procedure called hysterosalpingography (HSG). During an HSG, a special liquid that can be seen on X-rays is injected into the uterus through the cervix. This allows doctors to see the inside of the uterus and the fallopian tubes on the X-ray images. HSG is considered to be very accurate in determining if the fallopian tubes are open or not, with about 90% agreement when compared to another procedure called laparoscopic dye pertubation. However, even if the fallopian tubes appear to be open on the HSG, it does not guarantee that the eggs will be picked up by the tubes. For instance, women with severe endometriosis may have their ovaries stuck in a certain area of the pelvis, even though their fallopian tubes are normal.
During the follicular phase, ultrasound evaluation is conducted to identify certain conditions that may contribute to unexplained infertility, such as uterine fibroids, polyps, and congenital cavitary anomalies like a septate uterus. This initial assessment also provides information on ovarian volume and antral follicle counts, which are crucial in the investigation of infertility. To fully evaluate the uterine cavity, additional procedures may be required. Sonohysterography, for instance, involves using ultrasound and introducing sterile water to assess conditions like uterine polyps, submucus leiomyomas, or Asherman’s syndrome (uterine synechiae). Another option is diagnostic office hysteroscopy, which allows for direct visualization of the uterine cavity.
How Laparoscopy Can Help Diagnose Unexplained Infertility
The role of laparoscopy in investigating infertility has evolved over the past ten years. It used to be a routine part of infertility evaluations, but now it is only used in specific cases. Laparoscopy is a preferred method because it allows doctors to directly examine the reproductive organs in the pelvis. This test is particularly useful in identifying hidden factors that affect fertility, such as endometriosis and pelvic adhesions. The American Society for Reproductive Medicine (ASRM) recommends that laparoscopy be performed in women with unexplained infertility, those showing signs of endometriosis, or those suspected of having reversible adhesive tubal disease.
Tips for Conducting a Comprehensive Evaluation of Unexplained Infertility
It is recommended that couples undergo various tests to determine the cause of their infertility. These tests include a semen analysis, ovulation detection (using mid luteal progesterone and LH kit), assessment of ovarian reserve, transvaginal ultrasound, and HSG. By conducting these comprehensive tests, it is found that only a small percentage of couples, ranging from 15% to 30%, will be diagnosed with unexplained infertility.
Treatment of Unexplained Infertility

When all the recommended tests fail to identify any abnormalities, doctors diagnose unexplained infertility. Since there is no specific defect or functional impairment to address, the treatment for unexplained infertility is considered empirical. There are several treatment options available for unexplained infertility, including expectant observation with timed intercourse and lifestyle changes, clomiphene citrate and intrauterine insemination (IUI), controlled ovarian hyperstimulation (COH) with IUI, and in vitro fertilization (IVF). In this article, we will discuss the different treatment strategies, highlighting their advantages and disadvantages.
Managing Expectations and Making Lifestyle Adjustments: Dealing with Unexplained Infertility
Studies have shown that smoking, having an unhealthy body mass index (BMI), and consuming excessive amounts of caffeine and alcohol can reduce a woman’s fertility. It is recommended that women with a high BMI work towards achieving a normal weight, limit their caffeine intake to no more than 250 mg per day (equivalent to two cups of coffee), and restrict their alcohol consumption to no more than four standard drinks per week.
Couples with unexplained infertility have a lower chance of getting pregnant without any treatment compared to fertile couples, but the chances are still greater than zero. It is possible that unexplained infertility is just at the lower end of the normal range of fertility, with no actual defect present. However, it is also possible that the standard infertility tests may miss subtle defects due to imperfect or incomplete methods. Research on couples with unexplained infertility who are not receiving any treatment has shown a wide range of pregnancy rates over time. One study reviewed 45 different studies and found that the average chance of getting pregnant per cycle ranged from 1.3% to 4.1% in the untreated groups, which is lower than most treatment options. Another recent study in the Netherlands found that couples with unexplained infertility who were waiting for in vitro fertilization (IVF) had a cumulative chance of 10% to 15%.
The effectiveness of operative laparoscopy in improving pregnancy outcomes for individuals with unexplained or minimal/mild endometriosis remains a topic of debate. In a study conducted in 1997, Marcoux and colleagues conducted a randomized controlled trial involving 341 infertile women aged 20 to 39 with minimal or mild endometriosis. During the diagnostic laparoscopy, the women were randomly assigned to undergo either resection or ablation of visible endometriosis or diagnostic laparoscopy alone. The participants were then followed for 36 weeks after the laparoscopy procedure, or up to 20 weeks of pregnancy if they became pregnant during that time. The results showed that in the intervention group, 50 out of 170 women became pregnant during the follow-up period, while only 29 out of 169 women in the diagnostic laparoscopy group achieved pregnancy. This corresponded to fecundity rates of 4.7 and 2.4 per 100 person-months, respectively (rate ratio, 1.9; 95% confidence interval, 1.2–3.1).
IUI
Intrauterine insemination involves the placement of washed sperm into the uterine cavity around the time of ovulation. It can be performed in conjunction with natural ovulation timed with LH kit, ovulation induction using clomiphene citrate, or injectable gonadotropins. Few data exist on the use of IUI without ovarian hyperstimulation (OH). In 1991, Kirby and colleagues reported a RCT of 73 couples with unexplained infertility who were either randomized to IUI or timed intercourse. Conceptions occurred in 6 of 145 (4.1%) of the IUI cycles and 3 of 123 (2.4%) of the timed intercourse cycles. A large RCT showed that intracervical insemination alone had lower pregnancy rates per couple compared with IUI alone. It has been estimated that 37 cycles of IUI without additional ovarian stimulation would be needed to obtain an additional pregnancy compared with control cycles. A recent Cochrane review on this topic confirmed that IUI with ovulation induction increased the live birth rate compared with IUI alone. Therefore, IUI without additional treatment with clomiphene citrate or gonadotropins is not routinely performed in couples with unexplained infertility.

COH and IUI
n recent years, there has been a noticeable rise in the utilization of Controlled Ovarian Hyperstimulation (COH) as a treatment for unexplained infertility. COH involves the use of medications like clomiphene citrate and gonadotropins, either with or without Intrauterine Insemination (IUI). The idea behind COH is that it can potentially address subtle ovulatory issues that may have been missed during standard testing. By increasing the number of eggs available for fertilization, the chances of achieving pregnancy may also be enhanced. Similarly, IUI can play a role by introducing washed sperm directly into the uterus, thereby increasing the concentration of motile sperm available to fertilize the ovulated eggs.
Research studies have examined the impact of performing intrauterine insemination (IUI) on two consecutive days compared to a single IUI. However, these trials have been challenging to interpret due to the inclusion of patients with different types of infertility, including male factor and cervical factor, not just unexplained infertility. While some studies have suggested slight advantages of double IUI, the most recent randomized trial concluded that there is no significant difference in outcomes between single and double IUI for patients undergoing controlled ovarian hyperstimulation (COH)/IUI. Consequently, double IUI is not routinely offered.
IVF/ICSI
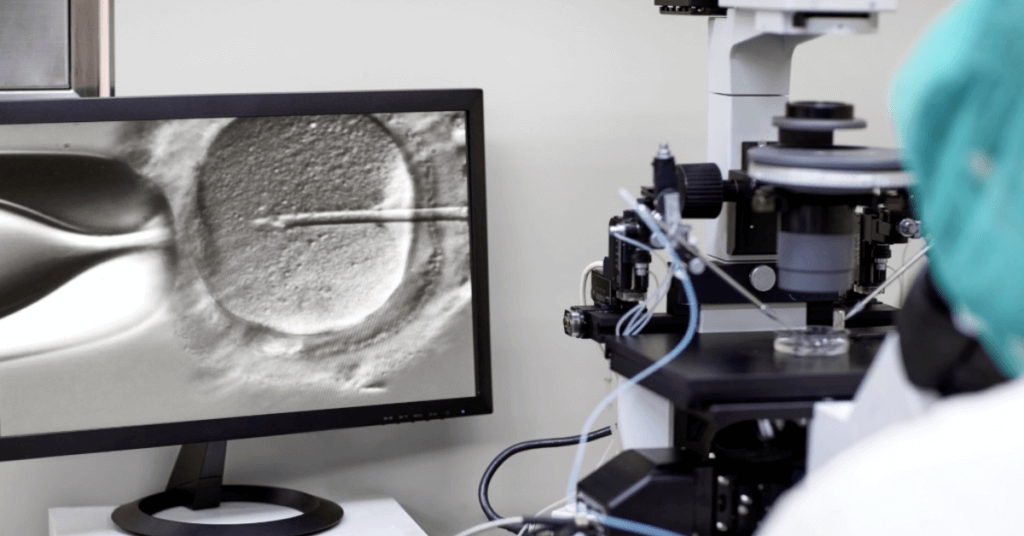
Assisted reproductive technology, such as IVF, is the most expensive but also the most effective treatment for unexplained infertility. It is often chosen when other less costly options have been unsuccessful. According to the 2006 SART data, there were 126,726 completed cycles for unexplained infertility, with a live birth rate of 40.4% for women under 35 and 38.9% for women aged 35 to 37. IVF not only offers the highest success rate but can also provide an explanation for infertility in some couples. Some IVF programs may perform ICSI in all couples with unexplained infertility, while others may only do so in 50% of cases.
Comparing Various Methods for Treating Unexplained Infertility
A randomized trial has not been conducted to compare the different treatment options for unexplained infertility. In a study by the European Society for Human Reproduction and Embryology (ESHRE) Multicentre Trial in 1991, it was found that the pregnancy rates per cycle were 15.2% for gonadotropin-only cycles, 27.4% for gonadotropin and IUI cycles, and 25.7% for IVF cycles. Over time, the pregnancy rate for IVF cycles has increased due to advancements in media, embryo micromanipulation, and extended embryo culture. The ASRM Practice Committee analyzed previously published data to determine the appropriate roles and cost-effectiveness of different procedures for managing unexplained infertility. Limited information is available regarding the cost-effectiveness of various treatments, but there seems to be a correlation between treatment cost and success.
A recent study called the FASTT Trial compared two different approaches to treating unexplained infertility. The study involved 503 couples who were randomly assigned to either a conventional treatment plan or an accelerated plan. All couples had unexplained infertility and were undergoing infertility treatment for the first time. The conventional treatment plan consisted of three cycles of clomiphene citrate/IUI, three cycles of FSH/IUI, and up to six cycles of IVF. On the other hand, the accelerated treatment plan involved three cycles of clomiphene citrate/IUI followed by up to six cycles of IVF. In total, 247 couples in the conventional group received 646 clomiphene citrate/IUI cycles, 439 FSH/IUI cycles, and 261 IVF cycles. Meanwhile, the accelerated group included 256 couples who received 642 clomiphene citrate cycles and 357 IVF cycles. As of April 2007, 18.5% of the women in the conventional group had experienced positive outcomes.
Summary and Conclusions
A thorough but time-efficient investigation of the infertile couple is required prior to a diagnosis of unexplained infertility. Couples should undergo a semen analysis, ovulation testing, assessment of ovarian reserve, and imaging to assess for tubal and uterine factors before a diagnosis of unexplained infertility is made. This workup can be completed within 1 menstrual cycle. In the couples with unexplained infertility, various treatment modalities are available, including expectant management with lifestyle changes, operative laparoscopy, COH (clomiphene citrate or gonadotropins) with IUI, and IVF (with or without ICSI). The optimal treatment strategy needs to be based on individual patient characteristics such as age, treatment efficacy, side-effect profile such as multiple pregnancy, and cost considerations.
Main Points
- Before a diagnosis of unexplained infertility is given, it is important for couples to undergo various tests. These tests include semen analysis, ovulation testing, assessment of ovarian reserve, and imaging to evaluate the condition of the fallopian tubes and uterus.
- The main options for treating unexplained infertility are: closely monitoring and having sex at the right time, making lifestyle changes, using clomiphene citrate and intrauterine insemination (IUI), undergoing controlled ovarian hyperstimulation with IUI, or trying in vitro fertilization (IVF).
- Expectant management is the least expensive option but has the lowest success rates in helping couples with unexplained infertility. It may be suitable for couples where the woman is young and there are no immediate concerns about running out of eggs.
- The treatment of unexplained infertility that is both expensive and highly effective involves assisted reproductive technology, such as IVF. IVF is considered the best option for unexplained infertility when other less expensive treatments have been unsuccessful.
- When deciding on the best course of action for treating unexplained infertility, it is important to consider the unique qualities of each patient. These qualities include age, how effective the treatment is, potential side effects like multiple pregnancies, and the cost of the treatment.




