Have you ever wondered why some couples struggle with multiple miscarriages during the first trimester of pregnancy? It’s a heart-wrenching experience that affects countless individuals worldwide. Miscarriage, defined as the loss of a fetus before 20 weeks gestation, can occur for various reasons. However, today we will focus specifically on possible causes for multiple miscarriages occurring between 6-8 weeks, and how they can impact the chances of achieving a live birth.
The first trimester is an incredibly delicate period in which the embryo develops into a tiny little baby. At this stage, preimplantation and early pregnancy complications, such as infertility and fibroids, can arise, leading to unexpected outcomes. One possible cause of recurrent early pregnancy loss is a septate uterus, a condition related to reproductive endocrinology, where a wall or band divides the uterus partially or completely. This congenital condition increases the risk of miscarriage due to inadequate space for proper fetal development, affecting the chances of a successful live birth.
Emotionally, experiencing multiple miscarriages, especially during a third pregnancy, can be devastating for couples who are eagerly anticipating the arrival of their little one. The joy and excitement quickly turn into grief and confusion as they grapple with repeated losses and unanswered questions related to infertility and molar pregnancy. It’s crucial for these couples to seek medical advice promptly after each incident in the first trimester to identify any underlying issues that may contribute to their recurrent losses.
Fortunately, there are support resources available for individuals coping with multiple miscarriages, including those experiencing problems with a third pregnancy or infertility. Support groups provide an outlet for sharing experiences and finding solace in knowing others have faced similar challenges, especially for those who have gone through molar pregnancies. Healthcare professionals specializing in reproductive medicine can offer guidance, conduct necessary tests, and explore potential treatment options tailored to each couple’s unique situation.
In this blog post series on multiple miscarriages at 6-8 weeks, we will delve deeper into the causes behind these losses, including the potential impact of a third pregnancy and molar pregnancy. We will also discuss common symptoms such as bleeding and how ultrasound can play a crucial role in diagnosis and monitoring. Our aim is to provide valuable information that empowers individuals going through this difficult journey while shedding light on important aspects often overlooked.
Stay tuned as we navigate through the complexities surrounding recurrent early pregnancy loss, including the challenges of a third miscarriage and a second miscarriage. We will discuss the importance of ultrasounds and how bleeding can be a concerning symptom. Together, let’s explore these difficult experiences.
Early Miscarriages at 6-8 Weeks: Causes and Factors:

Common causes of early miscarriages, such as chromosomal abnormalities
One of the most common causes of early miscarriage is chromosomal abnormalities. These abnormalities can occur during fertilization or when the embryo starts developing. When there are errors in the chromosomes, it can lead to an unsuccessful pregnancy. This can be particularly devastating for women who have experienced a second or third miscarriage, as they may be more prone to bleeding during these early stages.
Chromosomal abnormalities, such as bleeding, can be caused by genetic mutations or errors in cell division. These scan issues may arise randomly or be inherited from one or both parents. The abnormal chromosomes prevent the embryo from developing properly and often result in a miscarriage.
It’s important to note that early miscarriages, such as a second or third miscarriage, can occur naturally due to chromosomal abnormalities. These abnormalities are usually not preventable and are a matter of chance and genetics. They do not indicate any wrongdoing on the part of the mother or father. Additionally, experiencing bleeding during an early miscarriage is common.
Impact of maternal age on the risk of multiple miscarriages
Maternal age plays a significant role in the risk of experiencing multiple miscarriages at 6-8 weeks, especially if there is bleeding. As women age, their eggs also age, increasing the chances of chromosomal abnormalities and other complications during pregnancy.
Women over the age of 35 have a higher risk of experiencing recurrent early miscarriages compared to younger women. This is because older eggs are more likely to have genetic defects that can lead to unsuccessful pregnancies.
While it’s important to remember that every woman is different and these risks vary individually, medical professionals often recommend additional testing for women who have experienced multiple miscarriages after the age of 35. These tests help identify any underlying issues that may contribute to recurrent pregnancy loss.
Role of lifestyle factors, such as smoking and excessive alcohol consumption
Lifestyle factors can also play a significant role in early miscarriages at 6-8 weeks. Smoking cigarettes and excessive alcohol consumption have been linked to an increased risk of miscarriage.
Cigarette smoke contains harmful chemicals that can negatively affect the developing embryo and placenta. It can reduce blood flow to the uterus, leading to complications and potential miscarriages. Similarly, excessive alcohol consumption during pregnancy is known to cause fetal alcohol syndrome and increase the risk of miscarriage.
To minimize the risk of early miscarriages, it’s crucial for women who are trying to conceive or are already pregnant to avoid smoking altogether and limit their alcohol intake or abstain from it completely. Making these lifestyle changes can significantly improve the chances of a successful pregnancy.
Influence of hormonal imbalances in early pregnancy loss
Hormonal imbalances can also contribute to the loss of a pregnancy at 6-8 weeks, including the third miscarriage. Hormones play a crucial role in maintaining a healthy pregnancy by regulating various processes within the body.
Imbalances in hormones such as progesterone and estrogen can disrupt the normal development of the embryo and lead to miscarriage. Insufficient levels of progesterone, for example, may prevent the uterus from properly supporting the embryo, making it difficult for implantation and successful pregnancy.
Identifying hormonal imbalances requires medical evaluation through blood tests and other diagnostic methods. In some cases, hormone replacement therapy or other treatments may be recommended to address these imbalances and increase the chances of carrying a pregnancy successfully.
Understanding Recurrent Pregnancy Loss:

Definition and Diagnosis Criteria for RPL
Recurrent pregnancy loss (RPL) refers to the unfortunate experience of multiple miscarriages at 6-8 weeks gestation. It is a distressing condition that affects many women around the world. To be diagnosed with RPL, a woman typically needs to have experienced two or more consecutive pregnancy losses.
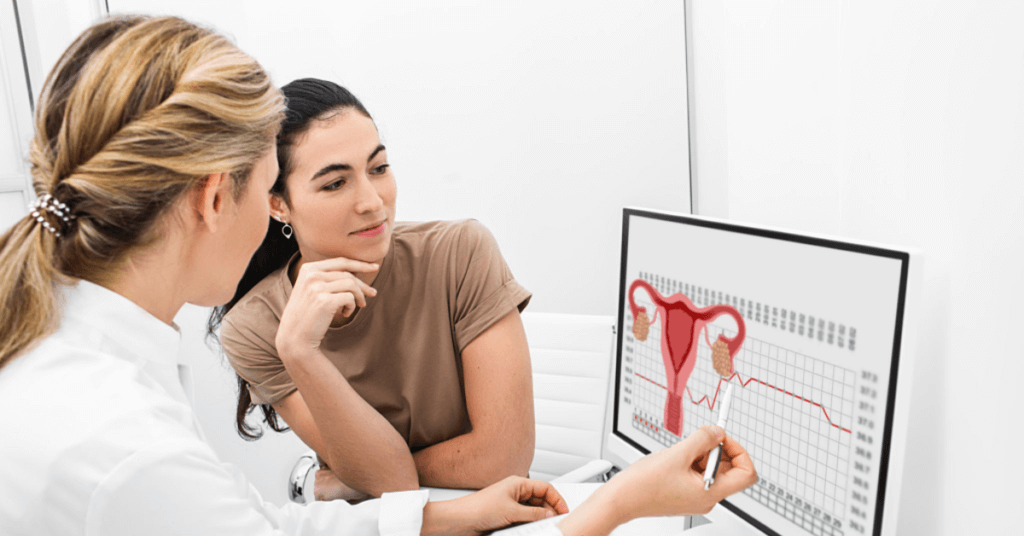
The diagnosis of RPL involves a thorough evaluation by specialists in reproductive endocrinology. They will consider various factors such as maternal age, medical history, genetic factors, uterine abnormalities, hormonal imbalances, and autoimmune disorders. This comprehensive assessment helps determine the underlying causes of recurrent pregnancy loss and guides appropriate treatment options.
Frequency and Statistics Related to RPL Cases Worldwide
Recurrent pregnancy loss is unfortunately not uncommon. Approximately 1-2% of couples trying to conceive experience this heartbreaking phenomenon. The frequency may vary across different populations and regions worldwide due to various genetic, environmental, and lifestyle factors.
In terms of statistics, it is estimated that around 75% of all pregnancies result in live births, while the remaining 25% end in pregnancy losses. Among these losses, about 1-5% are classified as recurrent pregnancy loss cases. These numbers highlight the significance of addressing this issue and providing support for individuals going through such difficult experiences.
Psychological Effects on Women Experiencing Recurrent Pregnancy Loss
Experiencing multiple miscarriages can have profound psychological effects on women. The emotional toll can be overwhelming as they navigate feelings of grief, sadness, guilt, anger, and even depression. Each loss brings renewed anxiety and uncertainty about future pregnancies.
It is essential to acknowledge the emotional impact of recurrent pregnancy loss and provide adequate support systems for affected women. Counseling services specializing in reproductive health can help individuals cope with their emotions during this challenging time. Connecting with support groups or online communities where others share similar experiences can offer a sense of understanding and validation.
Importance of Comprehensive Medical Evaluation for RPL Patients
A comprehensive medical evaluation is crucial for individuals experiencing recurrent pregnancy loss. It is necessary to identify any underlying factors that may contribute to the losses and guide appropriate treatment strategies. The evaluation typically involves a series of tests, including genetic screening, blood work to assess hormone levels, imaging studies to examine the uterus, and assessments for autoimmune disorders.
By conducting a thorough assessment, healthcare professionals can tailor treatment plans based on the specific needs of each patient. This approach increases the chances of successful future pregnancies and provides reassurance for those affected by recurrent pregnancy loss.

Genetic Factors in Multiple Miscarriages:
Recurrent miscarriages can be a heartbreaking experience for couples who are eagerly trying to expand their family. While there can be various factors contributing to multiple miscarriages at 6-8 weeks, genetic abnormalities play a significant role in this unfortunate phenomenon. Understanding the genetic factors behind recurrent miscarriages is crucial in identifying potential causes and exploring available testing options.
Overview of genetic testing options for identifying potential causes of multiple miscarriages
Genetic testing can provide valuable insights into the underlying causes of recurrent miscarriages. It involves analyzing the genetic material of both parents to identify any abnormalities that may contribute to pregnancy loss. One such option is preimplantation genetic testing (PGT), which is performed on embryos before they are transferred during an IVF procedure. PGT helps identify chromosomal abnormalities in embryos, enabling doctors to select genetically normal embryos with higher chances of successful implantation and reducing the risk of miscarriage.
Another type of genetic testing used in cases of recurrent miscarriage is karyotyping. This test examines the chromosomes of both parents to determine if there are any structural or numerical abnormalities that could lead to pregnancy loss. By analyzing the karyotype, healthcare providers can identify specific chromosomal alterations that may increase the risk of miscarriage.
Role of parental chromosomal abnormalities in recurrent early pregnancy loss
Parental chromosomal abnormalities can significantly contribute to recurrent early pregnancy loss. These abnormalities occur when there are changes or errors within the chromosomes carried by either parent’s reproductive cells (sperm or eggs). Chromosomes carry our genetic information, and any imbalances or defects can disrupt normal fetal development, leading to miscarriage.
For instance, certain conditions like translocations involve rearrangements of genetic material between different chromosomes. If one parent carries such a translocation, it increases the likelihood that their embryo will have an abnormal number or arrangement of chromosomes, resulting in a higher risk of miscarriage.
Link between inherited genetic disorders and increased risk of miscarriage
Inherited genetic disorders can also play a role in the occurrence of multiple miscarriages. Some genetic conditions are known to increase the risk of pregnancy loss due to their impact on fetal development. For example, women with blood clotting disorders, such as Factor V Leiden mutation or antiphospholipid syndrome, may experience recurrent miscarriages because these conditions can interfere with proper blood flow to the developing fetus.
Certain inherited genetic disorders can lead to an increased likelihood of producing aneuploid cells. Aneuploidy refers to an abnormal number of chromosomes in a cell, which can occur due to errors during cell division. Embryos with aneuploid cells often fail to implant properly or result in early pregnancy loss.
It is worth noting that other factors like uterine abnormalities (such as fibroids) and hormonal imbalances can also contribute to recurrent miscarriages. However, focusing on the genetic aspect is crucial for understanding potential causes and exploring appropriate treatment options.
Hyperactive Immune System and its Role in Miscarriages:
How an Overactive Immune System Can Contribute to Repeated Early Pregnancy Losses
Having a hyperactive immune system can be a significant factor in multiple miscarriages occurring at 6-8 weeks. The immune system is designed to protect the body from harmful invaders, such as bacteria and viruses. However, when it becomes overactive, it can mistakenly identify the developing embryo as a foreign substance and launch an attack on it.
In some cases, women with an overactive immune response may produce antibodies that target the fetus. These antibodies can interfere with the normal development of the pregnancy and lead to miscarriage. Chronic inflammation caused by an overactive immune system can create an unfavorable environment for implantation and further increase the risk of early pregnancy loss.
The Role Inflammation Plays in Increasing the Risk
Inflammation plays a crucial role in increasing the risk of miscarriage in cases where there is hyperactivity of the immune system. When inflammation occurs within the uterus, it can disrupt the delicate balance necessary for successful implantation and fetal development.
The presence of conditions like polycystic ovary syndrome (PCOS) or infections can trigger inflammation in the reproductive organs. This inflammatory response activates immune cells within these tissues, leading to damage to both maternal and embryonic tissue. As a result, this process interferes with normal implantation and increases the likelihood of miscarriage.
How Immune System Dysfunction Can Affect Implantation
Immune system dysfunction can significantly impact implantation during early pregnancy stages. Under normal circumstances, certain immune cells called regulatory T-cells help maintain tolerance towards fetal tissue by suppressing any harmful immune responses against it. However, when there is dysfunction or imbalance in these regulatory mechanisms, complications may arise.
An overactive immune response may cause excessive activation of natural killer (NK) cells within the uterus. These cells are responsible for recognizing and eliminating cells that they perceive as abnormal or foreign. In the case of pregnancy, if NK cells are excessively activated, they may target the developing embryo, leading to implantation failure and subsequent miscarriage.
Potential Treatments Targeting the Immune Response
Addressing immune system dysfunction can offer potential treatments to reduce the risk of multiple miscarriages at 6-8 weeks. Consulting with a specialist who specializes in reproductive immunology is crucial in identifying and managing immune-related factors contributing to recurrent pregnancy loss.
Some treatment options that may be considered include:
- Immunomodulatory therapies: Medications such as corticosteroids or intravenous immunoglobulin (IVIG) can help regulate an overactive immune response and reduce inflammation within the uterus.
- Anticoagulant therapy: Blood clotting disorders can contribute to early pregnancy losses. Anticoagulant medications like low molecular weight heparin may be prescribed to prevent blood clots from forming and improve blood flow to the placenta.
- Lifestyle modifications: Adopting a healthy lifestyle by maintaining a balanced diet, exercising regularly, managing stress levels, and avoiding harmful substances like smoking or excessive alcohol consumption can support overall immune health during pregnancy.
It is important to note that each individual’s situation is unique, and treatment plans should be tailored accordingly based on thorough evaluation by a specialist in reproductive immunology.
Autoimmune Diseases and their Impact on Pregnancy:
Autoimmune diseases, such as lupus and antiphospholipid syndrome, can have a significant impact on pregnancy, especially. These conditions are characterized by the body’s immune system mistakenly attacking healthy cells and tissues. When this happens during pregnancy, it can lead to complications that increase the risk of recurrent miscarriage.
Relationship between autoimmune diseases (e.g., lupus, antiphospholipid syndrome) and recurrent miscarriage
Women with autoimmune diseases, particularly lupus and antiphospholipid syndrome, are more prone to experiencing recurrent miscarriages. The reasons behind this association are multifaceted. In the case of lupus, autoimmunity can affect various aspects of pregnancy. It may disrupt the normal development of the placenta or cause inflammation in the blood vessels supplying nutrients to the fetus. This can result in poor fetal growth or even loss of pregnancy.
Antiphospholipid syndrome is another autoimmune disorder that significantly increases the risk of recurrent miscarriages. This condition leads to abnormal blood clotting due to antibodies targeting certain proteins found in cell membranes. These clots can obstruct blood flow to the developing fetus, leading to its demise.
Effectiveness of immunosuppressive therapies in reducing the risk
Immunosuppressive therapies have shown promise in reducing the risk of multiple miscarriages associated with autoimmune diseases. By suppressing an overactive immune response, these treatments aim to create a more favorable environment for a successful pregnancy.
In cases where lupus is involved, medications like corticosteroids or hydroxychloroquine may be prescribed to control inflammation and prevent flare-ups during pregnancy. These drugs help manage symptoms while minimizing potential harm to both mother and baby.
For women with antiphospholipid syndrome, treatment often involves blood-thinning medications such as low-dose aspirin or heparin. These drugs help prevent the formation of blood clots and improve blood flow to the developing fetus.
It is important to note that each case is unique, and treatment plans should be tailored to individual needs. Close collaboration between the patient, obstetrician, and rheumatologist or immunologist is crucial to determine the most appropriate course of action.
Importance of close monitoring during pregnancy for women with autoimmune conditions
Close monitoring throughout pregnancy is essential for women with autoimmune conditions, especially those who have experienced multiple miscarriages. Regular check-ups allow healthcare professionals to closely monitor both maternal and fetal health, making timely interventions when necessary.
Monitoring may involve regular ultrasounds to assess fetal growth and development. Blood tests can help identify any signs of disease activity or complications that may arise during gestation. By detecting potential issues early on, healthcare providers can take appropriate measures to ensure a safe and healthy pregnancy.
Potential complications associated with autoimmune diseases during gestation
Autoimmune diseases can pose various challenges during pregnancy, potentially leading to complications that require careful management. Some common complications include:
- Pre-eclampsia: Women with certain autoimmune disorders are at an increased risk of developing pre-eclampsia—a condition characterized by high blood pressure and organ damage—during pregnancy.
- Gestational diabetes: Autoimmune disorders such as lupus or thyroid disorders can contribute to the development of gestational diabetes—a temporary form of diabetes that occurs during pregnancy.
- Premature birth: Autoimmunity can increase the likelihood of premature labor, which carries its own set of risks for both mother and baby.
- Intrauterine growth restriction (IUGR): Poor placental function due to autoimmunity may result in inadequate nutrient supply to the fetus, leading to restricted fetal growth.
These potential complications highlight the importance of comprehensive prenatal care for women with autoimmune conditions. With proper monitoring and proactive management, the risks associated with these conditions can be minimized, increasing the chances of a successful pregnancy.
Less Common Reasons for Early Miscarriages:
Uterine Abnormalities: Not Your Typical Culprit
Most people assume that the underlying cause is related to chromosomal abnormalities or other common factors. However, there are instances where uterine abnormalities play a significant role in recurrent pregnancy loss.
Uterine abnormalities refer to structural irregularities within the uterus that can hinder successful implantation and development of an embryo. These abnormalities may include septate uterus (a condition where the uterus is divided by a wall), bicornuate uterus (a heart-shaped uterus), or unicornuate uterus (a one-sided uterus). In some cases, these abnormalities can lead to multiple miscarriages at 6-8 weeks.
While uterine abnormalities are relatively uncommon, they should not be overlooked when investigating the reasons behind recurrent early miscarriages. If you have experienced multiple miscarriages and suspect uterine abnormalities as a possible cause, consult with your healthcare provider who may recommend further evaluation through imaging tests such as ultrasound or hysteroscopy.
Infections and Sexually Transmitted Diseases: A Hidden Risk
Infections and sexually transmitted diseases (STDs) can pose a significant risk during early pregnancy and increase the chances of experiencing a miscarriage. While many people associate infections with later stages of pregnancy, they can also play a role in early pregnancy loss.
Certain infections such as bacterial vaginosis, urinary tract infections (UTIs), and sexually transmitted diseases like chlamydia or gonorrhea can lead to complications that affect fetal development. These conditions create an unfavorable environment for the embryo, making it difficult for it to thrive and grow properly.
It’s crucial to prioritize your sexual health before attempting conception if you have a history of multiple early miscarriages. Regular check-ups with your healthcare provider are essential for diagnosing and treating any underlying infections or STDs that could potentially impact your pregnancy.
Endocrine Disorders: Polycystic Ovary Syndrome (PCOS) and Beyond
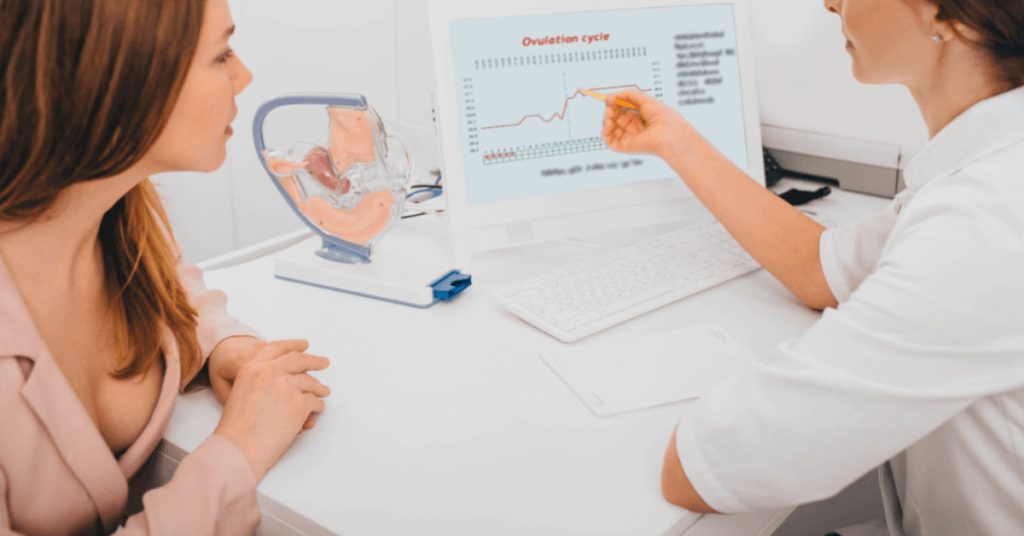
Endocrine disorders, such as polycystic ovary syndrome (PCOS), can also contribute to recurrent early miscarriages. PCOS is a hormonal disorder that affects the ovaries and disrupts normal ovulation. This condition is characterized by irregular menstrual cycles, high levels of male hormones (androgens), and the presence of small cysts on the ovaries.
The hormonal imbalances associated with PCOS can make it difficult for an embryo to implant properly in the uterine lining. These imbalances may lead to issues with egg quality, making it more challenging for a pregnancy to progress beyond the early stages.
If you suspect that an endocrine disorder like PCOS could be contributing to your multiple miscarriages, consult with a reproductive endocrinologist or fertility specialist. They can provide a comprehensive evaluation and develop a personalized treatment plan to optimize your chances of achieving a successful pregnancy.
Environmental Factors: The Unexpected Influencers
While chromosomal abnormalities are often considered the primary cause of early miscarriages, environmental factors should not be overlooked. Exposure to certain toxins and chemicals in our surroundings can increase the risk of experiencing recurrent miscarriages at 6-8 weeks.
Environmental factors that may impact early pregnancy include exposure to cigarette smoke, heavy metals (such as lead or mercury), pesticides, industrial chemicals, and radiation. These substances can interfere with fetal development and increase the likelihood of miscarriage.
To minimize potential risks from environmental factors, it’s advisable to adopt healthy lifestyle practices. Avoid exposure to harmful substances whenever possible, maintain good indoor air quality, eat a balanced diet rich in nutrients, exercise regularly, and practice stress management techniques.

Treatments to Increase Chances of a Successful Pregnancy:
Overview of Medical Interventions
Experiencing multiple miscarriages can be emotionally devastating for couples. However, there are several medical interventions available that can help increase the chances of a successful pregnancy. These treatments aim to address underlying conditions or factors that may have contributed to the recurrent miscarriages.
One common approach is assisted reproductive technologies (ART), which encompass various fertility treatments. ART includes procedures such as in vitro fertilization (IVF) and intrauterine insemination (IUI). IVF involves retrieving eggs from the ovaries, fertilizing them with sperm in a laboratory, and then transferring the resulting embryos into the uterus. This technique offers hope to couples struggling with infertility issues or recurrent miscarriages by increasing their chances of achieving a viable pregnancy.
Role of Assisted Reproductive Technologies
Assisted reproductive technologies play a significant role in improving pregnancy outcomes for couples facing multiple miscarriages. In cases where there are known issues with egg quality or quantity, IVF can be particularly beneficial. By directly retrieving eggs from the ovaries, fertility specialists can carefully select healthy eggs for fertilization, increasing the likelihood of successful embryo development.
Moreover, IVF allows for additional testing options that can provide valuable insights into potential causes of recurrent miscarriage. Preimplantation genetic testing (PGT) is one such option. PGT involves screening embryos for chromosomal abnormalities before they are transferred into the uterus. This helps identify embryos with a higher chance of implanting successfully and reduces the risk of another miscarriage.
Importance of Preconception Care
Before attempting another pregnancy, it is crucial for couples who have experienced multiple miscarriages to focus on preconception care and optimizing their overall health. This includes addressing any underlying medical conditions that could contribute to recurrent pregnancy loss.
A key aspect of preconception care is evaluating ovarian reserve – an indication of a woman’s egg quantity and quality. Fertility specialists can assess ovarian reserve through ultrasound and blood tests, providing insights into the chances of successful conception. Knowing this information allows couples to make informed decisions about the most effective treatment options.
Optimizing overall health involves ensuring both partners have healthy sperm and eggs. Lifestyle modifications, such as maintaining a balanced diet, regular exercise, managing stress levels, and avoiding harmful substances like tobacco and excessive alcohol consumption, can significantly improve fertility outcomes.
Potential Benefits and Risks
While fertility treatments offer hope for couples struggling with multiple miscarriages, it is essential to consider the potential benefits and risks associated with these interventions. The success rates of ART vary depending on several factors, including age, underlying condition, and previous pregnancy history.
It is crucial to discuss the potential risks with a healthcare provider before proceeding with any treatment. These may include multiple pregnancies (such as twins or triplets), ovarian hyperstimulation syndrome (OHSS) – a condition that causes enlarged ovaries due to fertility medications – or an increased risk of ectopic pregnancy.
However, it is important not to overlook the emotional toll that recurrent miscarriages can have on individuals or couples. Seeking support from mental health professionals or joining support groups can provide valuable assistance throughout the journey.

Navigating the Next Pregnancy After Multiple Miscarriages
Emotional challenges faced by couples when considering another pregnancy after multiple losses
Experiencing multiple miscarriages at 6-8 weeks can be an incredibly challenging and emotional journey for couples. The rollercoaster of hope, loss, and grief can take a toll on their mental well-being, making it difficult to consider embarking on another pregnancy. The fear of going through the pain of yet another loss may make them hesitant to try again.
During this time, it is crucial for couples to acknowledge and address their emotions. Seeking emotional support from loved ones, friends, or even professional counselors can provide a safe space for them to express their feelings and fears. Sharing these emotions with someone who understands can help alleviate some of the burden they carry.
Joining support groups or online communities specifically designed for individuals who have experienced multiple miscarriages can be immensely helpful. Connecting with others who have gone through similar experiences allows couples to share stories, gain insights, and find solace in knowing they are not alone.
Importance of seeking emotional support during subsequent pregnancies
When facing a third pregnancy after multiple miscarriages, seeking emotional support becomes even more critical. The lingering uncertainty from previous losses may create heightened anxiety throughout the entire process. Having a strong support system in place can provide comfort and reassurance during this time.
It is essential for partners to communicate openly about their fears and concerns regarding the new pregnancy. Sharing these worries with each other fosters understanding and strengthens their bond as they navigate this challenging journey together.
In addition to seeking support from loved ones, consulting with a healthcare professional specializing in reproductive health is highly recommended. Doctors experienced in managing pregnancies after recurrent miscarriages understand the unique needs of patients in such situations. They can offer guidance tailored specifically to each couple’s circumstances and provide reassurance throughout the process.
Role of close monitoring and specialized prenatal care in subsequent pregnancies
After experiencing multiple miscarriages, close monitoring and specialized prenatal care play a crucial role in subsequent pregnancies. Regular check-ups and ultrasounds can provide valuable insights into the progress of the pregnancy, offering reassurance to the couple.
In some cases, additional testing may be recommended to identify any underlying problems that could contribute to recurrent miscarriages. For instance, genetic testing can help determine if there are any chromosomal abnormalities or translocations that could increase the risk of future losses. Identifying these factors early on allows doctors to develop appropriate management plans for a healthier pregnancy.
Furthermore, healthcare providers may suggest specific interventions such as progesterone supplementation or blood-thinning medications to support a successful pregnancy. These measures aim to address potential issues identified during previous losses and improve the chances of carrying the baby full-term.
Coping strategies for managing anxiety and fear during a subsequent pregnancy
Managing anxiety and fear during a subsequent pregnancy after multiple miscarriages is vital for the well-being of both partners. Here are some coping strategies that can help:
- Educate yourself: Understanding common causes of miscarriage and learning about healthy lifestyle choices during pregnancy can empower you with knowledge and alleviate fears.
- Practice self-care: Engage in activities that promote relaxation and reduce stress levels, such as meditation, gentle exercise, or pursuing hobbies you enjoy.
- Communicate openly: Share your concerns with your partner, friends, or healthcare provider. Expressing your feelings can provide relief and create space for emotional support.
- Focus on positive affirmations: Remind yourself daily of your strength and resilience throughout this journey. Surround yourself with positive thoughts and affirmations to counteract negative emotions.
- Take it one day at a time: Pregnancy after multiple miscarriages often comes with increased uncertainty. Embrace each day as it comes while staying hopeful for a successful outcome.
Remember that every pregnancy is unique, and past experiences do not necessarily predict the future. By prioritizing emotional well-being, seeking support, and receiving specialized care, couples can navigate subsequent pregnancies after multiple miscarriages with increased confidence and hope for a healthy baby.

Managing Multiple Miscarriages at 6 Weeks
Experiencing multiple miscarriages at 6-8 weeks can be a devastating and emotionally challenging journey for women. While it may feel overwhelming, there are medical options, psychological support, and post-miscarriage care available to help manage these early losses effectively.
Medical Options for Managing Early Miscarriages at 6 Weeks Gestation
When faced with multiple miscarriages at 6 weeks gestation, it is crucial to consult with a healthcare professional who can guide you through the available medical options. Some of these options may include:
- Expectant Management: In some cases, your doctor may suggest allowing the body to naturally expel the pregnancy tissue without any intervention. This approach often involves close monitoring through weekly scans to ensure that the process is progressing as expected.
- Medications: Depending on your specific situation, your healthcare provider might prescribe medications such as misoprostol to help induce contractions and facilitate the passage of pregnancy tissue.
- Surgical Intervention: If necessary, surgical procedures like dilation and curettage (D&C) or suction aspiration may be recommended to remove any remaining tissue from the uterus.
It’s important to remember that each woman’s experience is unique, and what works for one person may not work for another. Discussing these medical options with your healthcare provider will help determine the most suitable course of action for you.
Psychological Support for Women Going Through Repeated Early Losses
The emotional toll of experiencing multiple miscarriages cannot be underestimated. It is essential to seek psychological support during this difficult time. Connecting with a therapist or counselor who specializes in reproductive loss can provide invaluable guidance and coping strategies.
Talking openly about your feelings with loved ones or joining support groups can also offer comfort and reassurance. Sharing experiences with others who have gone through similar situations can create a sense of belonging and understanding that aids in healing emotionally.
Remember, it is okay to grieve and take the time you need to process your emotions. Be gentle with yourself and seek support when necessary.
Importance of Follow-up Appointments and Post-Miscarriage Care
After experiencing a miscarriage, follow-up appointments with your healthcare provider are crucial. These check-ups allow for monitoring your physical recovery, ensuring that any potential complications are addressed promptly.
During these appointments, your doctor may conduct various tests to assess hormone levels, perform ultrasounds to confirm the complete passage of pregnancy tissue, or provide guidance on when it is safe to try conceiving again.
Post-miscarriage care also involves taking care of your emotional well-being. Your healthcare provider can offer resources and recommendations for additional support services that can help you navigate the grief and emotional healing process effectively.
Potential Complications or Risks Associated with Managing Multiple Miscarriages at 6 Weeks
While managing multiple miscarriages at 6 weeks gestation, there are potential complications or risks that you should be aware of:
- Incomplete Miscarriage: Sometimes, not all pregnancy tissue is expelled naturally or through medication. This situation may require further intervention such as a surgical procedure to prevent infection or other complications.
- Emotional Impact: Experiencing multiple miscarriages can have a profound emotional impact on women and their partners. Feelings of grief, anxiety, depression, and fear of future pregnancies are common during this time.
- Physical Recovery: It’s essential to give your body time to heal after each miscarriage before attempting another pregnancy. Rushing into conception without allowing sufficient recovery may increase the risk of subsequent miscarriages.
- Underlying Causes: Multiple miscarriages could be an indication of underlying medical conditions such as hormonal imbalances, genetic abnormalities, or structural issues in the reproductive system. Consulting with a specialist in recurrent pregnancy loss can help identify any potential causes and guide appropriate treatment options.
Remember that every woman’s journey is unique, and it’s crucial to work closely with your healthcare provider to develop a personalized plan that addresses your specific needs and concerns.
Managing multiple miscarriages at 6 weeks can be emotionally draining, but with the right medical support, psychological assistance, and post-miscarriage care, you can find the strength to heal and move forward.
Coping with Multiple Miscarriages at 8 Weeks:

Emotional Impact on Individuals Coping with Repeated Losses at 8 Weeks Gestation
Experiencing multiple miscarriages, especially at the 6-8 week mark, can be an incredibly challenging and emotionally draining journey. The loss of a pregnancy is a deeply personal and heartbreaking experience that can leave individuals feeling overwhelmed, devastated, and questioning their own bodies. It is important to acknowledge and validate these emotions while seeking support from loved ones and professionals.
The emotional impact of multiple miscarriages at 8 weeks gestation is unique to each person. Some may feel a sense of grief for the loss of what could have been, while others might experience anger or frustration towards their bodies for not being able to carry a pregnancy successfully. These feelings are completely valid and should not be dismissed or brushed aside.
During this difficult time, it is crucial to surround yourself with understanding and empathetic individuals who can offer support. Seeking out support groups or online communities where you can connect with others who have gone through similar experiences can provide a safe space for sharing feelings, fears, and coping strategies. Talking openly about your emotions can help alleviate some of the burden you may be carrying.
Support Systems Available for Those Experiencing Grief and Loss
When dealing with the pain of multiple miscarriages at 8 weeks gestation, it is essential to remember that you are not alone in this journey. There are several support systems available to help individuals navigate through their grief and find solace during this challenging time.
One valuable resource is professional counseling or therapy services specializing in reproductive loss. A trained therapist can provide guidance, empathy, and coping mechanisms tailored specifically for those experiencing repeated miscarriages. They can assist in processing complex emotions such as guilt, sadness, anxiety, or even depression that may arise from these losses.
Leaning on friends and family members who are understanding and compassionate can provide a much-needed support system. These loved ones can offer a listening ear, lend a shoulder to cry on, or simply be present during moments of vulnerability. Sharing your feelings with trusted individuals can help alleviate the sense of isolation that often accompanies grief.
Strategies for Self-Care During the Healing Process
While grieving the loss of multiple pregnancies at 8 weeks gestation, it is crucial to prioritize self-care and establish healthy coping strategies. Taking care of your physical and mental well-being can aid in the healing process and promote emotional resilience.
- Allow yourself to grieve: Give yourself permission to mourn the loss and acknowledge your emotions without judgment. It is essential to honor your feelings and not rush through the grieving process.
- Seek professional help: Consider reaching out to a therapist who specializes in reproductive loss or grief counseling. They can provide valuable tools and techniques tailored specifically for your needs.
- Practice self-compassion: Be gentle with yourself and practice self-compassion during this difficult time. Treat yourself with kindness, understanding that you are going through a challenging experience.
- Engage in activities that bring joy: Find solace in activities that bring you happiness and peace. Whether it’s engaging in hobbies, practicing mindfulness or meditation, or spending time in nature, allow yourself moments of respite from grief.
- Connect with others: Reach out to support groups or online communities where you can connect with individuals who have experienced similar losses. Sharing stories, fears, and coping strategies can foster a sense of belonging and provide comfort knowing you are not alone.
The Importance of Open Communication Within Relationships
Multiple miscarriages at 8 weeks gestation can place strain on relationships as partners navigate their shared grief while also managing their individual emotions. Open communication becomes vital during this time as it allows both individuals to express their feelings, fears, and concerns honestly.
Creating an environment where open dialogue is encouraged can help partners feel supported and understood. It is essential to actively listen to one another without judgment, offering empathy and validation for each other’s experiences. Sharing the burden of grief can strengthen the bond between partners and foster a sense of solidarity.
In addition to communication, couples may consider seeking couples therapy or counseling as a way to navigate their grief together. Professional guidance can provide tools for effective communication, promote understanding, and help partners find ways to support each other through this challenging journey.
Remember, coping with multiple miscarriages at 8 weeks gestation is a deeply personal experience, and there is no right or wrong way to grieve. Each individual’s healing process will be unique, but by seeking support, practicing self-care, and fostering open communication within relationships, it is possible to find solace and move forward on the path towards healing.
Insights on Multiple Miscarriages at 9 Weeks:

Early Miscarriages at 6-8 Weeks: Causes and Factors:
Miscarriages can be devastating, especially when they occur multiple times. At around 6-8 weeks of pregnancy, the risk of miscarriage is higher. Understanding the causes and factors behind early miscarriages can provide valuable insights into this distressing experience.
Understanding Recurrent Pregnancy Loss:
Recurrent pregnancy loss refers to the occurrence of three or more consecutive miscarriages. It is important to recognize that multiple miscarriages at 6-8 weeks can be emotionally challenging for individuals and couples trying to conceive. Seeking support from healthcare professionals and loved ones is crucial during this difficult time.
Genetic Factors in Multiple Miscarriages:
Genetic factors play a significant role in multiple miscarriages. Chromosomal abnormalities in either the embryo or one of the parents can increase the likelihood of recurrent pregnancy loss. Consulting with a genetic counselor may help identify any underlying genetic issues and guide future decisions regarding conception.
Hyperactive Immune System and its Role in Miscarriages:
An overactive immune system can contribute to repeated miscarriages. When the immune system mistakenly identifies a developing fetus as a threat, it may trigger an inflammatory response that affects implantation or proper fetal development. Exploring potential immunological interventions with a healthcare professional might be beneficial for those experiencing recurrent pregnancy loss.
Autoimmune Diseases and their Impact on Pregnancy:
Certain autoimmune diseases, such as lupus or antiphospholipid syndrome, can significantly impact pregnancy outcomes. These conditions cause the immune system to attack healthy cells, including those involved in maintaining a successful pregnancy. Close monitoring by medical specialists experienced in managing autoimmune disorders is essential for individuals with these conditions who are planning to conceive.
Less Common Reasons for Early Miscarriages:
While genetic factors and immune system dysregulation are common causes of multiple miscarriages at 6-8 weeks, there are other less common reasons to consider. These may include structural abnormalities of the uterus, hormonal imbalances, or infections. Consulting with a healthcare professional can help identify and address these underlying issues.
Treatments to Increase Chances of a Successful Pregnancy:
There are various treatments available to increase the chances of a successful pregnancy after multiple miscarriages. These may include lifestyle modifications, such as maintaining a healthy weight and avoiding harmful substances. Medical interventions like hormonal therapy or assisted reproductive technologies could be considered based on individual circumstances.
Navigating the Next Pregnancy After Multiple Miscarriages:
Embarking on another pregnancy journey after experiencing multiple miscarriages can be daunting. It is crucial to seek emotional support and guidance from healthcare professionals who specialize in managing recurrent pregnancy loss. They can provide personalized care plans and monitor the progress closely to improve the chances of a successful outcome.
Managing Multiple Miscarriages at 6 Weeks:
Managing multiple miscarriages at 6 weeks requires comprehensive medical attention and emotional support. Working closely with healthcare providers who understand the unique challenges faced by individuals going through recurrent pregnancy loss is essential for optimal management.
Coping with Multiple Miscarriages at 8 Weeks:
Coping with multiple miscarriages at 8 weeks can be overwhelming emotionally and physically. It is important to remember that everyone’s journey is different, and seeking professional counseling or joining support groups can provide comfort during this difficult time.
Remember that you are not alone in this experience. Reach out for support from your healthcare team, loved ones, or online communities specializing in recurrent pregnancy loss. Together, you can navigate through this challenging period and find hope for future pregnancies.
FAQs
Q: How long should I wait before trying again after multiple miscarriages?
After experiencing multiple miscarriages, it is recommended to consult with your healthcare provider regarding an appropriate timeframe for attempting another pregnancy. Factors such as physical recovery, emotional readiness, and any underlying causes of the miscarriages will influence this decision. Your healthcare provider will be able to provide personalized guidance tailored to your specific situation.
Q: Are there any lifestyle changes that can reduce the risk of multiple miscarriages?
Maintaining a healthy lifestyle can potentially reduce the risk of multiple miscarriages. This includes adopting a balanced diet, avoiding smoking and excessive alcohol consumption, managing stress levels, and maintaining a healthy weight. Discussing these lifestyle modifications with your healthcare provider is advisable for personalized recommendations.
Q: Can stress cause multiple miscarriages?
While stress alone may not directly cause multiple miscarriages, it can contribute to overall health imbalances that may increase the risk. Chronic stress affects various bodily systems, including hormonal regulation and immune function, which are crucial for successful pregnancies. Managing stress through relaxation techniques, counseling, or other appropriate interventions may be beneficial in reducing the chances of recurrent pregnancy loss.
Q: Is it possible to have a successful pregnancy after experiencing multiple miscarriages?
Yes, many individuals go on to have successful pregnancies after experiencing multiple miscarriages. With proper medical care and emotional support, identifying and addressing underlying causes can significantly improve the chances of a successful outcome. It is important to work closely with healthcare providers specializing in recurrent pregnancy loss for personalized care plans.
Q: What are some additional resources available for support during this challenging time?
There are several resources available for support during this difficult journey. Online communities dedicated to individuals experiencing recurrent pregnancy loss can provide valuable emotional support and shared experiences. Seeking professional counseling from therapists specializing in reproductive health or joining local support groups can also offer comfort and guidance throughout the process.




