
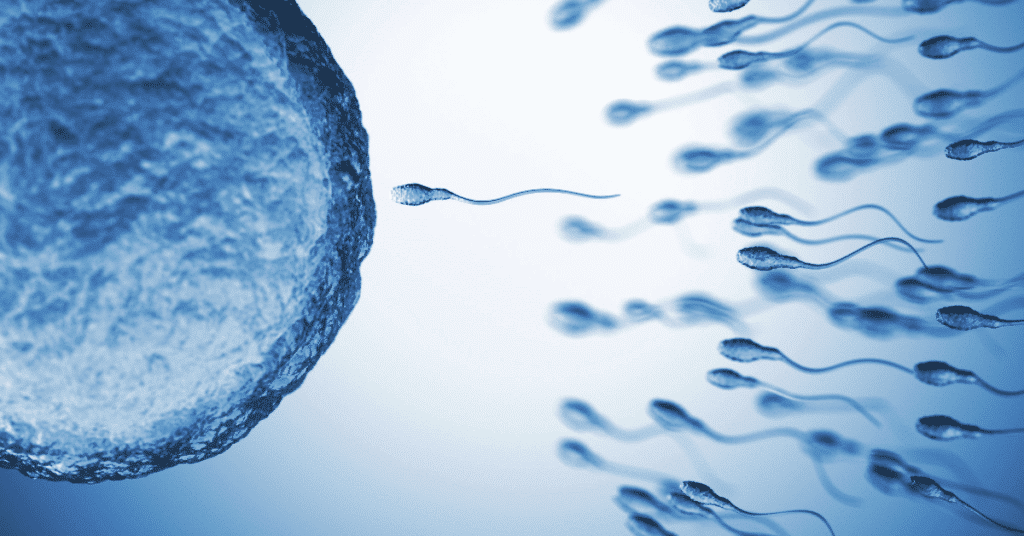
Have you ever wondered how couples struggling with male infertility can still have a chance at starting a family? Well, the answer lies in a groundbreaking procedure called intracytoplasmic sperm injection (ICSI) in the standard IVF laboratory. This remarkable technique has revolutionized fertility treatments and given hope to countless intended parents by injecting sperm directly into fertilized eggs, resulting in viable embryos.
Intracytoplasmic sperm injection (ICSI) is an assisted reproductive technology specifically designed to address male infertility. Unlike traditional IVF, where many sperm compete to fertilize an egg, ICSI involves injecting a single sperm directly into the egg’s cytoplasm. This precise method ensures that even men with low sperm count or poor motility can achieve successful fertilization. ICSI is commonly used when fertilized embryos or fertilized eggs are needed, and it can be performed after a semen analysis to determine the best course of action. Additionally, the hormone chorionic gonadotropin may be administered to stimulate egg production.
The procedure of icsi embryos takes place within the controlled environment of an IVF laboratory. Using a specialized needle, skilled embryologists delicately inject a single sperm into each mature egg during the icsi cycle. This intricate process requires precision and expertise to ensure optimal fertilization rate.
ICSI is particularly recommended for cases of male infertility caused by issues such as vasectomy or abnormal semen parameters. By directly introducing viable sperm into the egg’s cytoplasm in the standard IVF laboratory, this technique overcomes obstacles that would otherwise prevent conception for intended parents.
So if you find yourself facing challenges on your journey towards parenthood due to male infertility, rest assured that advancements like ICSI (intracytoplasmic sperm injection) offer new possibilities. With this innovative procedure, dreams of starting a family can become reality for many couples who never thought it possible before. ICSI allows for the direct injection of live sperm into the egg, increasing the chances of fertilization and the creation of a fertilized egg.
Remember:ICSI is the technique that’s changing lives.
Stay tuned to learn more about the steps involved in the standard IVF process and how it can bring joy to those longing for a child. Discover how live sperm is used during the ICSI process to fertilize the egg and create an embryo. Find out what happens in the following weeks after the procedure.
Understanding the ICSI Procedure:

The ICSI procedure, also known as intracytoplasmic sperm injection, is a crucial component of in vitro fertilization (IVF) treatment. This advanced technique requires specialized equipment and skilled embryologists to achieve successful outcomes. Let’s delve into the intricacies of the ICSI process and explore why it offers a higher chance of fertilization compared to conventional IVF. If you are undergoing IVF, consult your healthcare provider or doctor to learn more about this beta procedure and its benefits. It typically takes around two weeks for the entire ICSI process to be completed.
ICSI as part of IVF Treatment
In vitro fertilization, commonly used for couples experiencing fertility issues, involves combining an egg with sperm outside the body in a laboratory setting. This technique is performed by a healthcare provider and is beneficial for those facing problems such as low sperm count, poor sperm motility, or blocked fallopian tubes. Within the realm of IVF treatment, the doctor plays a vital role in overcoming specific male infertility problems, using techniques like ICSI.
The Specialized Equipment and Skilled Embryologists
Performing an ICSI procedure necessitates cutting-edge technology and expertise from trained embryologists, who are healthcare providers specializing in reproductive health for men. These professionals possess extensive knowledge in handling delicate reproductive cells and are adept at manipulating them under a microscope. Equipped with micromanipulation tools like microinjectors and high-magnification microscopes, they ensure precision during each step of the process.
Selecting and Immobilizing Healthy Sperm
During ICSI, healthcare providers meticulously choose a healthy sperm from the male partner’s semen sample. The selected sperm must exhibit optimal morphology (shape), motility (movement), and vitality to maximize the chances of successful fertilization. Once identified, the chosen sperm is immobilized using specialized techniques before being injected directly into an egg.
Monitoring Fertilization and Embryo Development
After injecting the selected sperm into an ICSI embryo, embryologists closely monitor its progress for signs of successful fertilization during the ICSI cycle. This entails observing cell division and embryo development under controlled laboratory conditions. By carefully tracking these crucial milestones, healthcare providers can determine if implantation of split ICSI embryos is likely to occur successfully.
Higher Chance of Fertilization
One of the key advantages of ICSI over conventional IVF is its significantly higher success rate in achieving fertilization for men. By manually injecting a single sperm directly into an egg, men’s chances of successful fertilization are greatly enhanced. This technique proves particularly beneficial when dealing with male infertility factors such as low sperm count or poor motility. As a healthcare provider, it’s important to consider ICSI as a viable option for men struggling with fertility issues.
Purpose and Benefits of ICSI:

Overcoming Male Infertility Issues
ICSI, or Intracytoplasmic Sperm Injection, is a groundbreaking procedure that has revolutionized fertility treatments. It serves as a lifeline for couples struggling with male infertility issues such as low sperm count or poor motility. In traditional IVF procedures, the sperm and egg are combined in a dish and left to fertilize naturally. However, when the male partner’s sperm quality is compromised, this method may not yield successful results. That’s where ICSI comes into play.
With ICSI, embryologists can handpick a single healthy men sperm and directly inject it into the egg using micromanipulation techniques. This precise procedure bypasses any barriers caused by low men sperm count or poor motility, giving couples a renewed hope of conceiving their own biological children. By providing an effective solution to male infertility challenges, ICSI opens up new possibilities for couples who previously faced limited options.
A Solution for Severe Male Factor Infertility
For some couples dealing with severe male factor infertility, conceiving a child through natural means may seem impossible. However, thanks to advancements in reproductive technology like ICSI, they now have a chance to fulfill their dreams of becoming parents. The ability to select and inject a single healthy sperm directly into the egg allows even those with significant fertility obstacles to experience the joy of parenthood.
By offering an alternative route to conception, ICSI provides hope for individuals who might otherwise have had no recourse but third-party reproduction methods such as donor insemination or adoption. It gives them an opportunity to conceive using their own genetic material and share that unique bond with their child, utilizing their own sperm cells.
A Second Chance After Failed IVF Attempts
In some cases, couples may have already undergone multiple unsuccessful attempts at traditional IVF before considering ICSI as an option. These failed attempts can be disheartening and emotionally draining for hopeful parents-to-be. However, ICSI offers a glimmer of hope in such situations.
By directly injecting the sperm into the egg, ICSI bypasses any potential obstacles that may have hindered fertilization during previous IVF cycles. This significantly reduces the risk of failed fertilization and increases the chances of achieving a successful pregnancy. Couples who have experienced disappointment and frustration from unsuccessful IVF attempts can find renewed optimism through ICSI.
Enhanced Pregnancy Success for Male Infertility
Male infertility can be a challenging hurdle for couples trying to conceive. However, with ICSI, the chances of achieving a successful pregnancy increase significantly. By directly injecting a healthy sperm into the egg, this procedure ensures that fertilization occurs even when traditional methods may have failed.
The ability to split and select sperm through split ICSI gives couples struggling with male infertility issues an advantage in their fertility journey. It maximizes their chances of creating embryos that are more likely to implant successfully in the uterus and lead to a healthy pregnancy.
Step 1: Ovarian Stimulation:
Ovarian stimulation is a crucial step in the ICSI procedure, as it plays a vital role in increasing the chances of successful fertilization and pregnancy. This phase involves using medications to promote multiple egg production in the ovaries, thereby maximizing the potential for successful IVF/ICSI treatment.
During the ovarian stimulation phase, a series of hormonal injections are administered over several days to stimulate follicle growth in the ovaries for icsi embryos. These injections contain specific hormones that mimic the natural process of egg development. The dosage and duration of these injections are carefully determined by a reproductive endocrinologist based on individual patient needs for split icsi.
Regular monitoring through ultrasounds and blood tests is essential during this phase of ICSI embryos to ensure optimal timing for egg retrieval. Ultrasounds help evaluate the growth and development of follicles within the ovaries of ICSI embryos, while blood tests measure hormone levels to assess ovarian response in ICSI embryos. Adjustments to medication dosage may be made throughout this phase of ICSI embryos based on these monitoring results.
The primary goal of ovarian stimulation is to increase the number of available eggs for fertilization during IVF/ICSI treatment. By stimulating multiple follicles to develop into mature eggs, there is a higher likelihood of obtaining viable embryos for transfer. This increases the chances of achieving pregnancy and ultimately helps couples struggling with fertility issues realize their dream of starting or expanding their family.
To initiate this important step in your fertility treatment cycle, you will typically start ovarian stimulation on day two or three of your menstrual cycle. The exact timing for split ICSI and ICSI embryos may vary depending on your specific treatment plan and medical history, which will be discussed with your reproductive endocrinologist.
Step 2: Retrieval and Preparation of Eggs:
After the initial step of ovarian stimulation, it’s time for the crucial process of retrieving and preparing the eggs. This step is essential to ensure that only mature and healthy eggs are used for the ICSI procedure. Let’s dive into the details of this important stage.
Egg retrieval procedure
The egg retrieval procedure is a minor surgical intervention that takes place in a medical facility under sedation or anesthesia. It involves using a thin needle to collect mature eggs from the ovaries. To access the ovaries, the doctor guides the needle through the vaginal wall.
Collecting mature eggs
Once inside, the needle carefully retrieves mature eggs from each ovary. These eggs are then immediately placed in a culture medium, which provides an optimal environment for their preparation. The culture medium mimics conditions similar to those found in a woman’s body, allowing the eggs to thrive outside of it.
Discarding immature or damaged eggs
During this process, any immature or damaged eggs are discarded. Only healthy and fully developed eggs are selected for further use in ICSI. This ensures that only high-quality eggs have a chance of being fertilized successfully.
Quick procedure with minimal discomfort
Egg retrieval is typically a quick procedure that lasts about 20-30 minutes. Although it may sound intimidating, rest assured that it is generally well-tolerated by patients due to anesthesia or sedation provided during the process.
The discomfort experienced during egg retrieval varies from person to person but is generally minimal. Some women may feel slight cramping or pressure in their pelvic region afterward, which can be managed with over-the-counter pain relievers if needed.
The laboratory dish journey
Once retrieved and prepared, these precious mature eggs embark on their journey towards fertilization. They are placed in a laboratory dish containing special nutrients and kept at an ideal temperature until they meet with sperm during ICSI.
The process of swimming and fertilization
Within a few hours, the sperm is injected directly into each mature egg using a microscopic needle. This technique, known as intracytoplasmic sperm injection (ICSI), increases the chances of successful fertilization. By bypassing any potential barriers, ICSI ensures that even if there are issues with sperm motility or morphology, fertilization can still occur.
Waiting for the next day
After the eggs have been injected with sperm, they are carefully monitored overnight. During this time, embryologists keep a close eye on their development. They observe whether fertilization has taken place and monitor the growth of embryos as they progress through different stages.
Breaking through the outer layer
The following day, embryologists check to see if fertilization has occurred successfully. They examine whether the embryos have managed to break through their outer layer called the zona pellucida. This outer layer protects the embryo during its early development stages but needs to be penetrated for implantation to occur later on.
Step 3: Obtaining Sperm Sample:
Obtaining a sperm sample is an essential step in the process. This involves collecting live and healthy sperm that will be used for fertilization. Let’s take a closer look at how this crucial stage is carried out.
Methods of Obtaining Sperm Sample
There are two primary methods for obtaining a sperm sample: ejaculation and surgical extraction techniques. In most cases, ejaculation is the simplest and most common method. The male partner will provide a semen sample through masturbation into a sterile container. This sample is then evaluated through semen analysis to determine its quality, quantity, and sperm count.
However, there may be instances where the male partner has low sperm count or no sperm present in their ejaculate due to various reasons such as male factor infertility. In such situations, surgical methods like testicular sperm extraction (TESE) may be employed. TESE involves extracting small tissue samples from the testicles using local anesthesia. These samples are then examined in the laboratory to identify viable sperm cells.
Laboratory Processing and Selection
Once the sperm sample is obtained, it undergoes laboratory processing to separate healthy and motile sperm from other components of semen such as seminal fluid and non-motile or abnormal sperm cells. This process helps ensure that only the best-quality sperm are used for ICSI.
Before selecting a suitable candidate for fertilization, further assessment of the collected sample takes place. The quality and quantity of the live sperm are carefully evaluated by fertility specialists through various parameters including motility, morphology, DNA integrity tests, and others depending on specific clinic protocols.
It’s important to note that during ICSI treatment, only one viable and high-quality sperm cell is needed for each egg being fertilized. Therefore, meticulous selection ensures optimal chances of successful fertilization while minimizing potential risks or complications associated with using suboptimal samples.
Step 4: Fertilization through ICSI
In the journey towards successful pregnancy, the ICSI procedure plays a crucial role. This step involves the delicate process of injecting a single selected sperm directly into each mature egg using a microneedle. Let’s dive deeper into what happens during this fascinating stage.
The Injection Process: Ensuring Successful Fertilization
One of the primary reasons for opting for ICSI is to overcome infertility issues related to natural sperm penetration of the egg’s outer layer, known as the zona pellucida. By bypassing this potential barrier, ICSI ensures that fertilization can occur even in cases where standard IVF techniques may not be effective.
During the procedure, an embryologist carefully selects a healthy and motile sperm under high magnification. This chosen sperm is then immobilized and drawn into a thin hollow needle, which is skillfully maneuvered to delicately pierce through the zona pellucida and inject the sperm directly into the egg’s cytoplasm. This precise technique guarantees that fertilization takes place successfully.
Monitoring for Successful Fertilization
After injection, close monitoring becomes essential to confirm whether fertilization has occurred within 24 hours. The embryologists at fertility clinics employ various methods to assess successful fertilization rates. They examine the eggs under a microscope to observe important indicators such as pronuclei formation – which signifies that both maternal and paternal genetic material have merged – as well as other cellular changes that confirm successful fertilization.
By closely observing these developmental milestones, fertility specialists can determine which embryos are most viable for further development and potential transfer back into the woman’s uterus.
From Fertilized Eggs to Viable Embryos
Once fertilized through ICSI, these eggs undergo further development and transform into embryos over several days. Skilled embryologists meticulously monitor their growth and progression in specialized laboratory conditions.
The goal is to nurture these fertilized eggs into viable embryos that have the best chance of resulting in a successful pregnancy. The development and quality of the embryos are assessed based on various factors, including cell division rates, cellular morphology, and overall appearance.
Throughout this critical stage, fertility clinics employ state-of-the-art technology and adhere to stringent protocols to ensure optimal conditions for embryo development. By providing the necessary support and maintaining an ideal environment, fertility specialists maximize the chances of achieving a successful pregnancy.
Step 5: Embryo Development and Monitoring:
Embryo development is a crucial stage in the ICSI procedure. Once fertilization occurs, the embryologist takes charge of culturing the embryos in a controlled laboratory environment. This carefully regulated setting provides optimal conditions for their growth and development.
The embryologist closely monitors the embryos over several days to assess their progress and quality. It’s like having your very own personal cheerleader rooting for your little potential bundle of joy! They keep a close eye on each embryo to ensure it reaches specific developmental milestones before being considered for transfer or cryopreservation (freezing).
Why is this monitoring so important, you ask? Well, it helps identify which embryos are viable and have higher chances of implantation and pregnancy success. The embryologist checks for signs of healthy development, such as reaching the blastocyst stage. This stage is a significant milestone where the embryo has developed into a more advanced structure with distinct cell types.
Imagine these embryos as little superheroes preparing themselves for an epic battle inside your womb! They need to be strong enough to withstand all the challenges that lie ahead. Continuous monitoring allows us to select those superheroes with the best chances of success.
Once selected, these mighty embryos are ready for transfer or cryopreservation. Transfer involves placing them back into your womb in hopes of achieving pregnancy. Cryopreservation, on the other hand, involves freezing them until you’re ready to embark on this incredible journey.
But how do we know if one of these superhero embryos has successfully implanted itself? That’s where pregnancy tests come into play! A pregnancy test measures beta hCG levels in your body. Beta hCG is a hormone produced by pregnant women, indicating that an embryo has implanted itself in the uterus.
After undergoing an ICSI procedure, waiting for that positive pregnancy test can be nerve-wracking yet exciting at the same time. It’s like waiting for Santa Claus on Christmas Eve, hoping for the best gift ever!
Once pregnancy is confirmed, you’ll embark on a beautiful journey towards motherhood. Regular ultrasounds and check-ups will help monitor the growth and development of your baby. These appointments allow healthcare professionals to detect any potential birth defects or complications early on.
Finally, after months of anticipation, the day arrives when you get to hold your precious little bundle of joy in your arms. The birth of a baby is a magical moment that fills your heart with indescribable joy and love. All those sleepless nights and endless worries melt away as you gaze into their innocent eyes.
Remember, each step in the ICSI procedure plays a vital role in helping couples achieve their dream of having a baby. The dedicated work done by embryologists in the laboratory ensures that only the strongest embryos are chosen for transfer or cryopreservation.
So, let’s raise our glasses to these unsung heroes who work tirelessly behind the scenes to make dreams come true! Cheers to science and miracles!
Additional Resources:
- Embryo Development: From Conception to Pregnancy
- What Is Beta hCG?
- Understanding Ultrasound Results During Pregnancy
- [Cryopreservation: Freezing Embryos, Eggs & Sperm](https://resolve.
Step 6: Embryo Transfer:
Embryo transfer is a crucial step in the ICSI procedure, where one or more carefully selected fertilized embryos are placed into the woman’s uterus using a thin catheter. This simple and relatively painless procedure is typically performed without anesthesia and does not require hospitalization.
The number of embryos transferred during this stage depends on several factors, including the woman’s age and the quality of the embryos. The aim is to maximize the chances of successful implantation while minimizing the risk of multiple pregnancies. For younger women with high-quality embryos, transferring fewer embryos may be recommended to reduce the likelihood of multiple births. On the other hand, older women or those with lower-quality embryos may benefit from transferring more embryos to enhance their chances of achieving pregnancy.
After the embryo transfer, it is common for women to be advised to rest for a short period before resuming normal activities. This rest period allows time for any potential discomfort or cramping to subside and gives the embryo(s) an opportunity to settle in the uterus. While there is no strict bed rest requirement, some clinics suggest avoiding vigorous exercise or heavy lifting during this time.
Following embryo transfer, patients often experience a mix of emotions ranging from excitement to anxiety as they await confirmation of pregnancy. Typically, a pregnancy test called beta-hCG (human chorionic gonadotropin) is conducted after a couple of weeks. This hormone, produced by cells that surround an implanted embryo, can be detected in blood or urine samples and indicates whether implantation has occurred.
It’s important to note that not all transferred embryos will successfully implant and result in pregnancy. The success rates vary depending on various factors such as maternal age, embryo quality, and overall health. However, advancements in technology have significantly improved these rates over time.
Results and Success Rates of ICSI:
ICSI, or intracytoplasmic sperm injection, has revolutionized fertility treatments for couples struggling with male infertility issues. This highly specialized procedure has significantly improved pregnancy rates, offering hope to those who may have previously felt discouraged. While success rates can vary based on various factors, such as maternal age and overall health, the average success rate of ICSI ranges from 40% to 50% per cycle.
Improved Pregnancy Rates for Couples with Male Infertility Issues

One of the most remarkable aspects of ICSI is its ability to overcome male infertility problems that would otherwise hinder natural conception. By directly injecting a single sperm into an egg, this procedure bypasses any obstacles presented by low sperm count, poor motility, or abnormal morphology. As a result, couples who were once deemed infertile due to male factors can now experience the joy of pregnancy.
Factors Affecting Success Rates
While ICSI offers promising results for many couples, it’s important to consider several factors that can influence the success rates. Maternal age plays a significant role in fertility outcomes. Women over the age of 35 generally have lower success rates compared to younger women due to declining egg quality and quantity. Underlying health conditions or lifestyle choices can impact the chances of a successful pregnancy.
The Percentage Game: Average Success Rates
When considering the effectiveness of ICSI, it’s essential to understand that success rates are reported as percentages per cycle attempted. On average, these rates range between 40% and 50%. However, it’s crucial to note that achieving a successful pregnancy may require multiple cycles in some cases. Each individual’s circumstances are unique; therefore, personalized information from a fertility specialist is invaluable when determining expected success rates.
Consulting with Fertility Specialists for Personalized Information
The decision to undergo any fertility treatment should be made in consultation with experienced professionals who can provide personalized guidance. Fertility specialists possess a wealth of knowledge and expertise in assessing individual factors that may influence the success of ICSI. By analyzing test results, considering medical history, and evaluating overall health, these specialists can offer realistic expectations regarding the chances of achieving pregnancy through this procedure.
The Journey to Success
Embarking on the path to parenthood through ICSI can be an emotional journey filled with hope and anticipation. It’s essential to approach the process with patience and understanding, as success rates are not guaranteed in every case. However, by working closely with a fertility specialist, couples can navigate the ups and downs of treatment while receiving the necessary support and guidance along the way.
Potential Risks and Considerations:
Risks Associated with ICSI Procedure
It’s important for couples to be aware of the potential risks and considerations involved. Like any medical procedure, ICSI carries several risks that need to be taken into account before making a decision. Here are some key points to note:
- Infection or Bleeding: As with any invasive procedure, there is always a risk of infection or bleeding at the injection site. Although these complications are rare, it’s essential to be aware of them. Your healthcare provider will take necessary precautions to minimize these risks.
- Damage to the Injected Egg: During the ICSI process, there is a small chance that the injected egg may get damaged. This can occur due to various factors such as improper handling or technical difficulties during the procedure. While this risk is minimal, it’s crucial to understand that it exists.
- Increased Risk of Genetic Abnormalities: Some studies have suggested a slightly increased risk of genetic abnormalities in children born through ICSI compared to natural conception or conventional IVF methods. However, it’s important to note that this risk remains relatively low overall.
Discussing Potential Risks with Your Healthcare Provider
Considering these potential risks and concerns associated with the ICSI procedure, it is highly advisable for couples contemplating this treatment option to have an open discussion with their healthcare provider beforehand. By doing so, they can gain a better understanding of their individual chances and make informed decisions about their fertility journey.
Your healthcare provider will guide you through the entire process and address any issues or questions you may have regarding potential complications or genetic problems associated with ICSI treatment. They will provide you with personalized advice based on your specific circumstances and medical history.
It’s important for couples undergoing fertility treatments like ICSI not only to consider the risks but also focus on maximizing their chances of success. Factors such as the quality of the eggs and sperm used, the experience and expertise of the medical team, and the number of attempts made can all influence the outcome.
The Impact and Future of ICSI:

The ICSI procedure has revolutionized the field of fertility treatment, offering hope to couples struggling with infertility. With its high success rates and ability to overcome various male factor infertility issues, ICSI has become a go-to option for many individuals seeking to start a family.
Understanding the ICSI Procedure:
ICSI stands for Intracytoplasmic Sperm Injection, a technique used in assisted reproductive technology (ART) that involves injecting a single sperm directly into an egg. This procedure is typically recommended when there are concerns about sperm quality or quantity.
Purpose and Benefits of ICSI:
The primary purpose of ICSI is to facilitate fertilization in cases where natural conception may be difficult or impossible. By bypassing potential barriers, such as low sperm count or poor motility, ICSI increases the chances of successful fertilization and embryo development.
Step 1: Ovarian Stimulation:
To enhance the chances of retrieving multiple eggs, women undergoing the ICSI procedure receive hormonal medications that stimulate their ovaries. This step aims to increase egg production for later retrieval.
Step 2: Retrieval and Preparation of Eggs:
Under ultrasound guidance, eggs are retrieved from the woman’s ovaries using a minimally invasive procedure called transvaginal oocyte retrieval. Once collected, these eggs are carefully prepared for fertilization by removing surrounding cells.
Step 3: Obtaining Sperm Sample:
A semen sample is collected from the male partner or donor through ejaculation. If necessary, techniques like testicular sperm extraction (TESE) can be used to retrieve viable sperm directly from the testicles.
Step 4: Fertilization through ICSI:
Using specialized micromanipulation equipment, a single sperm is injected directly into each mature egg obtained during retrieval. This precise technique ensures that fertilization occurs even if there are abnormalities in the sperm’s structure or movement.
Step 5: Embryo Development and Monitoring:
After fertilization, the embryos are cultured in a laboratory for several days. During this time, they are carefully monitored to assess their quality and development potential.
Step 6: Embryo Transfer:
Once the embryos have reached an optimal stage of development, they are transferred into the woman’s uterus. This procedure is typically performed using a thin catheter inserted through the cervix, aiming to achieve successful implantation and pregnancy.
Results and Success Rates of ICSI:
ICSI has shown remarkable success rates in achieving pregnancies, particularly in cases where male infertility factors are present. The overall success rate varies depending on various factors such as maternal age, egg quality, and underlying fertility issues.
Potential Risks and Considerations:
While ICSI offers hope to many couples struggling with infertility, it is important to be aware of potential risks associated with the procedure. These include an increased risk of multiple pregnancies, ovarian hyperstimulation syndrome (OHSS), and potential genetic concerns related to sperm abnormalities.
In conclusion, the ICSI procedure has revolutionized fertility treatment by offering a highly effective solution for couples facing male factor infertility challenges. Its ability to overcome barriers that hinder natural conception has provided countless individuals with the opportunity to fulfill their dreams of parenthood. If you or your partner are experiencing difficulties conceiving due to male infertility factors, exploring the option of ICSI may provide you with a promising path towards starting or expanding your family.
FAQs

Q: How successful is ICSI?
A: The success rate of ICSI varies depending on individual circumstances but generally ranges from 40% to 60% per cycle.
Q: Are there any long-term health risks associated with ICSI-conceived children?
A: Studies suggest that children conceived through ICSI do not face significantly higher health risks compared to naturally conceived children. However, long-term studies are ongoing.
Q: Can women with low ovarian reserve undergo ICSI?
A: Yes, women with low ovarian reserve can still undergo ICSI. However, the number of eggs retrieved may be limited, affecting the overall success rate.
Q: Is ICSI more expensive than traditional IVF?
A: The cost of ICSI is usually slightly higher than traditional IVF due to the additional laboratory procedures involved. It’s best to consult with your fertility clinic for accurate pricing information.
Q: Are there any lifestyle changes required after undergoing ICSI?
A: Following an ICSI procedure, it is generally recommended to maintain a healthy lifestyle, including regular exercise, a balanced diet, and avoiding smoking and excessive alcohol consumption.




