
Are you one of the many women who have experienced the heartbreak of recurrent miscarriages? Have you been diagnosed with impaired oocyte quality or diminished ovarian reserve, leaving you wondering about your reproductive potential and capacity? You’re not alone. Many women face these challenges in the field of reproductive medicine.
Miscarriage, also known as spontaneous abortion, is a devastating experience for any woman, especially for infertile women seeking reproductive medicine. But what happens when miscarriages become recurrent, happening time and time again due to uterine abnormalities? This is where the connection between diminished ovarian reserve and recurrent pregnancy losses, including biochemical pregnancies, becomes crucial.
Diminished ovarian reserve, also known as low ovarian reserve, refers to a decline in the quantity and quality of eggs in a woman’s ovaries. It can significantly impact fertility outcomes, making it harder for infertile women seeking assistance from a clinical infertility service to conceive naturally or through assisted reproductive techniques like IVF (in vitro fertilization). The reduced reproductive potential associated with low ovarian reserve poses unique obstacles for those trying to build their families, especially those who have experienced recurrent pregnancy losses. Women undergoing their first oocyte retrieval may also face challenges due to diminished ovarian reserve, as indicated by a lower antral follicle count.
Addressing the issue of diminished ovarian reserve is essential in reproductive medicine for infertile women. Understanding how this condition affects fertility allows healthcare providers to tailor treatments specifically for individuals facing this challenge, including those at higher miscarriage risk. From early pregnancy loss to failed oocyte retrieval during IVF cycles, exploring the implications of diminished ovarian reserve sheds light on the complexities surrounding infertility and the importance of addressing uterine abnormalities.
In this blog post series, we will delve into various aspects related to reproductive medicine, specifically diminished ovarian reserve and recurrent miscarriages. We’ll discuss its impact on fertility outcomes, including impaired oocyte quality, address common misconceptions, explore available treatment options such as first oocyte retrieval, and share stories of hope from women who have triumphed over these obstacles. Our focus will be on the importance of these topics in achieving higher pregnancy rates.
Join us as we uncover the mysteries behind diminished ovarian reserve in reproductive medicine and provide insights into navigating this journey towards parenthood for infertile women. Together, let’s empower ourselves with knowledge and support each other through these challenging times of infertility and impaired oocyte quality.
Impact of low ovarian reserve on miscarriage risk
Women who have been diagnosed with diminished ovarian reserve face unique challenges in reproductive medicine. The impact of low ovarian reserve on the risk of recurrent pregnancy losses is significant, and understanding this relationship is crucial for those affected by infertility.
Higher Risk of Recurrent Miscarriages
One of the key talking points regarding infertility is its association with recurrent miscarriages in women with low ovarian reserve. Research has shown that women with diminished ovarian reserve are more likely to experience multiple pregnancy losses. This can be an emotionally challenging journey for couples hoping to start or expand their families through reproductive medicine.
Miscarriage rates tend to increase as a woman’s oocyte quantity decreases in the context of infertility. With fewer oocytes available for fertilization, the chances of chromosomal abnormalities in embryos also rise. Chromosomal abnormalities are a leading cause of early pregnancy loss in the field of reproductive medicine, contributing to the higher risk experienced by women with low ovarian reserve, particularly those with polycystic ovary syndrome (PCOS).
Understanding the Impact on Early Pregnancy Loss
Another important aspect related to infertility and low ovarian reserve in reproductive age women is the increased risk of early pregnancy loss. Women with diminished ovarian reserve often face difficulties in achieving successful pregnancies due to lower oocyte quality and reduced fertility potential in the field of reproductive medicine.
Oocyte quality plays a significant role in determining pregnancy outcome in the field of reproductive medicine. As ovarian reserve declines, both the number and quality of eggs diminish, making it more challenging for fertilized embryos to implant successfully and develop into healthy pregnancies. This decreased fertility potential contributes to higher rates of early pregnancy loss among women with low ovarian reserve, which is a common concern in infertility and IVF treatments.
Exploring Reduced Fertility Potential and Miscarriage Rates
The relationship between recurrent pregnancy losses and infertility in women with polycystic ovary syndrome (PCOS) is complex but interconnected. When infertile women with diminished ovarian reserve have PCOS, their reproductive system may struggle to produce viable eggs regularly, leading to irregular menstrual cycles or even skipped periods. This can have a significant impact on pregnancy outcome.
These irregularities can make it difficult for infertile women trying to conceive naturally, increasing their reliance on assisted reproductive technologies such as in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI). While IVF can offer hope for young women with low ovarian reserve, it does not eliminate the risk of miscarriage. The quality of available oocytes still plays a crucial role in determining the success of the procedure and the likelihood of a healthy pregnancy.
Furthermore, research has shown that women with low antral follicle count (AFC), which is often associated with diminished ovarian reserve and low oocyte count, have higher miscarriage rates compared to those with normal AFC. This further emphasizes the impact of low ovarian reserve and low oocyte count on pregnancy outcomes.

Anti-Müllerian hormone as a risk factor for miscarriage
Anti-Müllerian hormone (AMH) levels can serve as an indicator for assessing miscarriage risk in women undergoing in vitro fertilization (IVF). Lower AMH levels are associated with an elevated chance of experiencing pregnancy loss. The role of AMH testing in predicting reproductive outcomes for women with diminished ovarian reserve, specifically oocyte count and serum AMH levels, is crucial in understanding their chances of successful pregnancies.
AMH Levels and Miscarriage Risk
One significant factor to consider is the level of Anti-Müllerian hormone (AMH) in a woman’s body. Research has shown that lower AMH levels are linked to a higher miscarriage risk. This means that women with diminished ovarian reserve, who typically have low serum AMH concentrations, may face increased challenges when trying to conceive and maintain a healthy pregnancy. IVF and PMOL can help address these challenges.
Several studies, including Lyttle Schumacher et al., have explored the relationship between müllerian hormone (AMH) levels and miscarriage risk. These findings highlight the importance of monitoring serum AMH concentrations as part of fertility assessments for women struggling with infertility or recurrent miscarriages. By identifying low AMH levels early on, healthcare professionals can provide appropriate interventions and support to improve the chances of a successful pregnancy, especially in women with normal ovarian reserve and concerns about ovarian aging. Additionally, monitoring AMH levels can help guide decisions regarding ovarian stimulation during fertility treatments.
Predicting Reproductive Outcomes with AMH Testing
In this context, investigating how müllerian hormone (AMH) levels influence the likelihood of having a successful pregnancy and IVF outcomes becomes crucial. Women with diminished ovarian reserve often experience difficulties conceiving due to decreased egg quantity and quality. By measuring serum AMH concentration through ultrasensitive AMH ELISA tests, doctors can gain insights into a woman’s ovarian reserve and predict her reproductive outcomes, including miscarriage risk and rates, more accurately.
AMH testing provides valuable information about a woman’s fertility potential, including her risk of miscarriage. It evaluates her antral follicle count (AFC), which refers to the number of small follicles present in the ovaries at any given time. AFC serves as an assessment of ovarian reserve and can indicate the likelihood of successful conception. Women with low AMH levels and a reduced AFC may face challenges in conceiving and maintaining a pregnancy, making it essential to consider alternative fertility treatments such as IVF.
The Role of AMH in Assisted Reproductive Technologies
High AMH levels can also present their own set of challenges for women undergoing in vitro fertilization (IVF) procedures. While women with high serum AMH concentrations may have an advantage in terms of ovarian reserve, they are at an increased risk of developing ovarian hyperstimulation syndrome (OHSS) during ART procedures. OHSS is a potentially dangerous condition that occurs when the ovaries overreact to fertility medications, resulting in enlarged ovaries and fluid accumulation. Recurrent pregnancy loss and miscarriage rates can also be affected by high AMH levels and may impact pregnancy outcomes.
To mitigate the risk of ovarian hyperstimulation syndrome (OHSS), doctors carefully monitor women with high anti-Müllerian hormone (AMH) levels during in vitro fertilization (IVF) cycles and adjust medication dosages for optimal ovarian stimulation and response. This helps optimize the chances of a successful pregnancy while minimizing miscarriage rates and ensuring the woman’s safety throughout the process.
Causes of Diminished Ovarian Reserve
Age: The Aging Factor
Age is a significant factor for young women. As we grow older over the years, our ovaries naturally age along with us. This physiological decline in ovarian function is a normal part of the aging process for infertile women and can lead to a decrease in both the quantity and quality of eggs produced, affecting pregnancy outcome.
When women are born, they already have their lifetime supply of eggs stored within their ovaries. However, as they age, this supply gradually diminishes, impacting pregnancy outcome and ivf success rates. Female age directly affects the number and quality of eggs available for fertilization, increasing the risk of miscarriage. As a woman approaches her late 30s and early 40s, her ovarian reserve begins to decline more rapidly, making it harder for her to conceive and increasing the likelihood of miscarriage.
Genetic Factors: A Role in Ovarian Function
Genetic factors can also contribute to reduced ovarian function and impaired oocyte quality, which can affect pregnancy outcome and increase miscarriage risk, especially for women undergoing IVF. Some women may inherit genetic variations that affect their egg development or cause premature depletion of their ovarian reserves, leading to higher miscarriage rates. These genetic factors can influence hormone levels, follicle growth, and overall reproductive health.
Understanding the role genetics play in pregnancy outcome and diminished ovarian reserve is crucial for diagnosing and managing this condition effectively. Genetic testing may be recommended for women experiencing fertility challenges or recurrent miscarriages associated with low ovarian reserve in the context of ivf. By identifying specific genetic markers or mutations related to diminished ovarian function, healthcare providers can provide targeted interventions or treatment options tailored to each individual’s needs based on the findings of a retrospective cohort study.
Medical Treatments: Unintended Consequences
Certain medical treatments, such as chemotherapy or radiation therapy used to treat cancer, can unintentionally impact ovarian reserves and increase miscarriage risk. These gonadotoxic treatments may damage the ovaries’ ability to produce healthy eggs, potentially affecting fertility potential and leading to premature menopause in low women.
If you have been diagnosed with cancer or are planning on undergoing gonadotoxic treatment, discussing ovarian stimulation and fertility preservation options with your healthcare provider is crucial. Techniques such as egg freezing or embryo cryopreservation can help preserve your fertility before undergoing ivf, increasing the chances of future successful pregnancies. It is also important to consider the potential miscarriage risk and the need for a pregnancy test after undergoing these procedures.
Autoimmune Conditions and Environmental Factors
Autoimmune conditions and environmental factors can also contribute to diminished ovarian function in low women. Autoimmune disorders, such as autoimmune oophoritis or primary ovarian insufficiency, can increase the ivf miscarriage risk by affecting the ovaries.
Environmental factors, including exposure to certain chemicals, pollutants, or toxins, may also impact ovarian health and increase the risk of miscarriage. Studies have suggested that prolonged exposure to environmental toxins like pesticides or heavy metals may have adverse effects on ovarian function and egg quality in IVF outcomes. Additionally, supplementation with DHEA has been shown to improve IVF outcomes.
While it may not be possible to control all environmental factors, being aware of potential risks and taking steps to minimize exposure can be beneficial for overall reproductive health. This is especially important when considering ovarian stimulation, as studies have shown that it can have an impact on outcomes such as miscarriage.
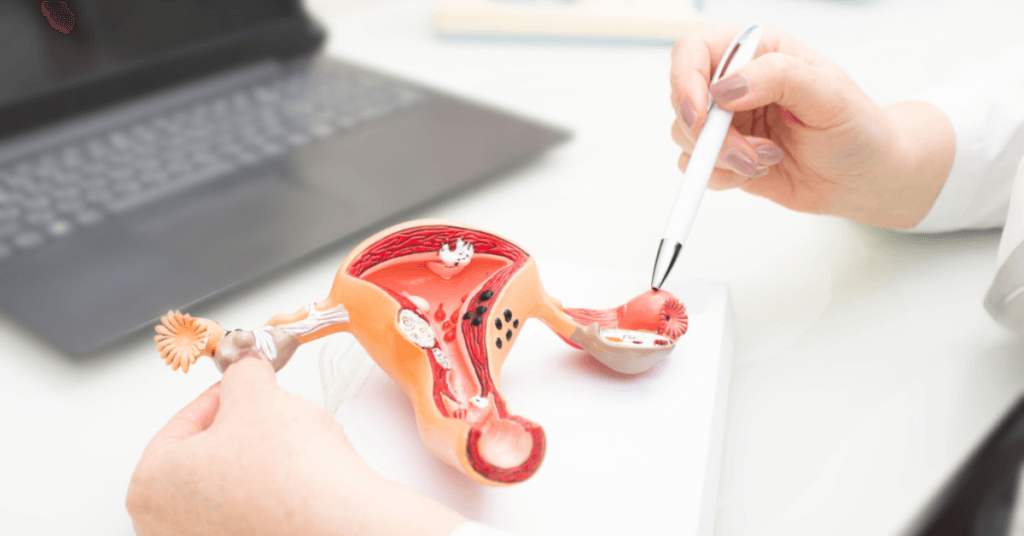
Relationship between diminished ovarian reserve and miscarriages
Women with diminished ovarian reserve (DOR) often face numerous challenges when trying to conceive, including an increased susceptibility to recurrent pregnancy losses. Understanding the relationship between DOR and miscarriages is crucial for those navigating the difficult journey of fertility. In a retrospective cohort study, it was found that women with DOR who underwent IVF had improved outcomes when taking dhea supplements. This study sheds light on the potential benefits of dhea in improving fertility in women with DOR.
Diminished ovarian reserve increases the susceptibility to recurrent pregnancy losses
Recurrent miscarriage, defined as the loss of two or more consecutive pregnancies before 20 weeks gestation, can be emotionally devastating for women and their partners. Research has shown that women with diminished ovarian reserve are at a higher risk of experiencing recurrent miscarriages. In a retrospective cohort study, it was found that women with diminished ovarian reserve had a higher likelihood of experiencing recurrent miscarriages. This finding highlights the importance of considering ovarian reserve in assessing the risk of recurrent miscarriage. Additionally, prospective studies are needed to further investigate the relationship between diminished ovarian reserve and recurrent miscarriage.
Diminished ovarian reserve, also known as low AMH, refers to a decline in both the quantity and quality of a woman’s eggs. As women age, their egg supply naturally diminishes, increasing the miscarriage risk. However, certain conditions or factors can accelerate this decline, such as genetic predisposition, medical treatments like chemotherapy or IVF, or autoimmune disorders.
When a woman’s egg quantity is reduced due to low anti-Müllerian hormone (AMH) levels and diminished ovarian reserve, it becomes more challenging for her body to produce healthy embryos capable of implanting and developing successfully. This decreased egg quantity may lead to chromosomal abnormalities in embryos, increasing the miscarriage risk for women undergoing in vitro fertilization (IVF).
Understanding how decreased egg quantity impacts embryo implantation and development
The number of eggs available for fertilization plays a critical role in determining the chances of successful conception, especially for low women undergoing IVF. With diminished ovarian reserve, there are fewer eggs available each menstrual cycle, which increases the miscarriage risk and reduces the likelihood of fertilization occurring during any given month, according to studies.
Moreover, even if fertilization does occur during in vitro fertilization (IVF), there is an increased risk of miscarriage. There have been studies that show an association between IVF and an elevated risk of miscarriage. Additionally, these studies have also found that embryos resulting from IVF have a higher likelihood of having chromosomal abnormalities. These abnormalities can hinder proper implantation into the uterine lining or disrupt normal embryonic development. Therefore, it is important for individuals undergoing IVF to be aware of these risks.
Embryo quality also plays an essential role in successful pregnancies, especially for women undergoing IVF. As egg quantity decreases with diminished ovarian reserve (DOR), so does oocyte quality – referring to the health and viability of individual eggs. Poor oocyte quality can result in embryos that are less likely to develop into healthy pregnancies, increasing the risk of miscarriage for medium and low women.
Exploring the link between poor oocyte quality and increased risk of spontaneous abortions
Women with low AMH levels, who are undergoing IVF due to their old age, may experience an increased risk of miscarriage. This is because as eggs age, they become more susceptible to genetic abnormalities, leading to early pregnancy loss.
The decline in egg quality associated with diminished ovarian reserve (DOR) may result from various factors, including oxidative stress and hormonal imbalances. Oxidative stress occurs when there is an imbalance between free radicals and antioxidants in the body, causing cellular damage. This oxidative stress can affect the quality of eggs in women undergoing in vitro fertilization (IVF) and increase the likelihood of miscarriages. A retrospective cohort study found that women with medium or low ovarian reserve may be particularly affected.
Hormonal imbalances, such as low AMH levels and elevated LH levels, can impact oocyte quality in women with low AMH. These imbalances disrupt the delicate hormonal environment necessary for optimal egg development and increase the risk of miscarriage in low AMH women undergoing IVF.
Discussing why women with low egg reserves may face challenges maintaining viable pregnancies
Women with low egg reserves often face a higher miscarriage risk. The reduced quantity and quality of eggs make it more difficult for these women to conceive naturally or through assisted reproductive technologies like in vitro fertilization (IVF). Numerous studies over the years have shown this medium.
Furthermore, even if conception does occur during in vitro fertilization (IVF), there is an increased risk of early pregnancy loss due to chromosomal abnormalities or impaired embryonic development. This heightened susceptibility to recurrent miscarriage adds emotional strain on couples already struggling with infertility. This information is supported by a retrospective cohort study and other relevant studies in the field.
It’s important for individuals facing challenges with fertility and IVF to seek support from medical professionals specializing in reproductive medicine. Studies have shown that personalized treatment options from fertility specialists can increase the chances of achieving a successful pregnancy, while also reducing the risk of miscarriage.

Detecting pregnancy and ascertainment of miscarriages
Early detection methods like home pregnancy tests can confirm pregnancy.
Home pregnancy tests are a convenient and accessible way to detect if you’re pregnant and assess the risk of miscarriage. These tests work by detecting the presence of human chorionic gonadotropin (hCG) hormone in your urine, which is crucial for conception and IVF success. Studies have shown that by simply collecting a small sample of urine on the test stick, you can find out if you’re carrying a little bundle of joy.
These tests are designed to be easy to use, even for those who aren’t medical professionals. You just need to follow the instructions provided with the test kit, which usually involves holding the absorbent tip under your urine stream or dipping it into a collected sample. Within minutes, the test will display either one line (indicating a negative result) or two lines (indicating a positive result). It’s important to note that false negatives can occur if you take the test too early in your pregnancy when hCG levels may still be low. These tests can help determine conception and assess miscarriage risk for those undergoing IVF treatment.
Ultrasound scans help in identifying viable pregnancies and detecting potential complications.
Ultrasound scans play a crucial role in monitoring pregnancies, including those resulting from IVF conception, and ensuring their healthy progression. These non-invasive imaging procedures use sound waves to create images of the inside of your body, including your uterus where the developing fetus resides. Studies have shown that ultrasound examinations are particularly important in detecting potential complications and reducing the risk of miscarriage. During an ultrasound examination, a trained technician or doctor will apply gel on your abdomen or insert a transvaginal probe to obtain clear images.
In early pregnancy, ultrasound scans can help determine gestational age and detect potential abnormalities or complications that may affect both maternal and fetal health. These scans are especially important for women who have experienced a miscarriage or undergone IVF treatments. Studies have shown that ultrasounds are a reliable medium for tracking growth milestones and estimating due dates accurately.
If there are concerns about miscarriage in low women due to diminished ovarian reserve or previous pregnancy losses, ultrasound scans can provide reassurance by confirming the presence of an intrauterine pregnancy. Seeing a tiny heartbeat flicker on the screen can be a moment of relief for anxious parents-to-be undergoing IVF. However, it’s important to note that ultrasounds cannot predict or prevent all potential complications, and regular prenatal care is necessary to ensure a healthy pregnancy according to studies.
Monitoring hormone levels, such as beta-hCG, aids in assessing pregnancy viability.
Beta-human chorionic gonadotropin (beta-hCG) is a hormone produced by the placenta during pregnancy. Monitoring its levels can provide valuable insights into the viability of a pregnancy, especially in cases of miscarriage. In early pregnancy, beta-hCG levels rise rapidly and can be measured through blood tests, which are commonly used in IVF studies. These tests help healthcare providers assess if the pregnancy is progressing as expected, and can also be used to measure serum AMH levels.
Regular monitoring of beta-hCG concentration is crucial in IVF pregnancies. A significant increase in beta-hCG levels over time indicates a healthy and viable pregnancy, while stagnant or declining levels may suggest an impending miscarriage or other complications. Healthcare professionals can intervene promptly if necessary and provide appropriate care by monitoring beta-hCG levels through serum studies.
It’s important to keep in mind that individual variations exist in miscarriage and IVF studies. Your healthcare provider will interpret your specific results based on factors such as gestational age, any underlying conditions you may have, and the serum levels.
Investigating the role of progesterone levels in determining the risk of miscarriage.
Progesterone is a crucial hormone for maintaining a healthy pregnancy. It helps prepare the uterus for implantation and supports early fetal development. Low progesterone levels in the serum have been associated with an increased risk of miscarriage, particularly in women with diminished ovarian reserve or previous miscarriages. Studies have shown that IVF patients with serum progesterone levels below 10 pmol/L have a higher risk of miscarriage.
To evaluate progesterone levels during the first trimester, your healthcare provider may order specific blood tests. These tests measure the amount of progesterone serum in your bloodstream and help determine if supplementation is necessary to support the pregnancy. These tests are particularly important for women who have experienced a miscarriage or are undergoing IVF, as studies have shown a link between progesterone levels and successful pregnancies in these cases.
Supplementing with progesterone, either through oral medication or vaginal suppositories, can help maintain adequate levels and reduce the risk of miscarriage in women undergoing IVF. However, it’s important to note that progesterone supplementation may not be effective in all cases and should always be done under the guidance of a healthcare professional. Recent studies have shown that low serum progesterone levels can negatively impact IVF outcomes in women.
Chromosomal abnormalities and their link to miscarriage
Chromosomal abnormalities play a significant role in the occurrence of spontaneous miscarriages. Analyzing studies shows that these genetic errors during embryo formation can lead to pregnancy loss, causing immense heartache for hopeful parents. Understanding the connection between chromosomal abnormalities and miscarriage is crucial in shedding light on this complex issue.
Advanced maternal age is one factor that increases the risk of chromosomal abnormalities and subsequent miscarriages in women. As women get older, the quality of their eggs decreases, making them more prone to genetic disorders. Research studies conducted by Chang et al and Abdullah et al have shown a significant association between advanced maternal age, low AMH levels, and aneuploidy rates in embryos during IVF analysis over the years.
Retrospective analysis studies have shown that IVF genetic testing techniques are valuable tools in assessing the likelihood of experiencing a miscarriage due to chromosomal abnormalities. By analyzing DNA samples from couples trying to conceive, these tests can identify potential genetic disorders or anomalies that may hinder successful pregnancies. This information allows healthcare professionals to provide appropriate guidance and support tailored to each couple’s unique circumstances.
It is important to note that not all cases of chromosomal abnormalities are related to advanced maternal age. Other factors such as uterine abnormalities, congenital malformations, or family history of genetic disorders can also contribute to an increased risk of miscarriage. Therefore, comprehensive genetic testing should be considered for individuals or couples facing recurrent pregnancy loss or those with known risk factors, as indicated by retrospective studies on IVF and AMH levels.
In addition to understanding the impact of advanced maternal age on chromosomal abnormalities during embryo development, it is essential to recognize the various types of pregnancy loss associated with these genetic errors. Miscarriages can manifest as biochemical pregnancies (early losses detected through blood tests) or ectopic pregnancies (implantation outside the uterus). Both scenarios are often linked to chromosomal abnormalities during embryo development. This understanding is crucial for IVF patients, as AMH analysis and studies have shown that advanced maternal age can increase the risk of these genetic errors.
The emotional toll experienced by couples navigating recurrent miscarriages, especially during IVF cycles, cannot be overstated. The uncertainty surrounding each cycle brings about anxiety and heartbreak. However, retrospective studies and analysis of genetic testing can provide valuable insights into the underlying causes of these losses, offering a glimmer of hope and potential avenues for treatment or prevention.

Conclusion: Understanding how diminished ovarian reserve contributes to miscarriages
Diminished ovarian reserve, characterized by low women’s egg quantity and quality in the ovaries, can have a significant impact on the risk of experiencing miscarriages. The level of anti-Müllerian hormone (AMH), which reflects ovarian reserve, has been identified as a risk factor for miscarriage. IVF treatments can help increase the chances of successful pregnancy for women with low AMH levels.
Studies have shown that women with low ovarian reserve are more likely to experience chromosomal abnormalities in their eggs, which increases the risk of miscarriage. It is important to detect pregnancy early and quickly identify miscarriages in order to better understand the connection between diminished ovarian reserve and miscarriages. This is especially relevant for women undergoing IVF treatment.
It is essential to recognize that there are various causes of diminished ovarian reserve, including age, genetic factors, environmental influences, certain medical conditions or treatments such as IVF and miscarriage. By understanding these causes, low women can make more informed decisions regarding their fertility options for years.
In conclusion, it is clear that diminished ovarian reserve plays a significant role in contributing to the occurrence of miscarriages in low women. Studies have shown that early detection and proper management are vital for individuals facing this challenge. If you or someone you know is struggling with infertility or recurrent miscarriages due to diminished ovarian reserve, it is advisable to seek guidance from healthcare professionals specializing in reproductive medicine, such as those experienced in IVF.
FAQs
Q: Can I still get pregnant if I have diminished ovarian reserve?
While low ovarian reserve and miscarriage may reduce your chances of conceiving naturally, studies have shown that assisted reproductive technologies such as IVF can still offer hope for pregnancy. Consulting with a fertility specialist will help determine the best course of action based on your specific circumstances and serum levels.
Q: Are there any lifestyle changes that can improve my chances of getting pregnant with diminished ovarian reserve?
While lifestyle changes alone cannot reverse diminished ovarian reserve completely, maintaining a healthy weight, managing stress levels effectively, and avoiding smoking and excessive alcohol consumption may positively impact overall fertility health for women undergoing ivf. Studies have shown that low women who have experienced miscarriage may benefit from these lifestyle changes.
Q: Can hormone therapy help improve my chances of carrying a pregnancy to term?
Hormone therapy, such as ovarian stimulation, can be used in IVF to increase the number of eggs available for fertilization. However, it is important to discuss the potential risks of miscarriage and the benefits with your healthcare provider as each case is unique. AMH levels in serum can also be a factor to consider.
Q: Are there any alternative treatments or natural remedies that may help improve my ovarian reserve?
While some alternative treatments and natural remedies claim to improve ovarian reserve for IVF, their efficacy is not scientifically proven in studies. It is advisable to consult with a fertility specialist who can provide evidence-based guidance on appropriate treatment options for IVF and miscarriage.
Q: How soon should I seek medical assistance if I suspect diminished ovarian reserve?
A: If you have been trying to conceive for over six months without success and suspect diminished ovarian reserve, it is recommended to consult with a fertility specialist sooner rather than later. Early intervention can offer more treatment options and potentially better outcomes for women with low ovarian reserve who have been trying to conceive for years. It is important to seek help from a specialist who can provide guidance on IVF and address the emotional challenges that may arise after a miscarriage.
Note: The FAQs provided above are for informational purposes only. It is always best to consult with a qualified healthcare professional for personalized advice on IVF, miscarriage, and studies.




