
Cancer, a formidable adversary that affects millions worldwide, not only threatens lives but also brings forth a multitude of challenges in the field of clinical oncology. Among these challenges is the potential impact on a woman’s ability to conceive during pregnancy. The question that often arises is: does chemotherapy make you infertile? Today, we delve into this topic to shed light on the effects of cancer treatments, including immunotherapy drugs, on female fertility and the ovaries.
For women battling various types of cancers such as breast cancer or ovarian cancer, concerns about infertility and menopause symptoms are all too real. The powerful drugs used in chemotherapy can wreak havoc on the delicate balance of hormones and reproductive organs, including the ovaries. As a result, many women experience changes in their menstrual cycles, irregular periods, or even complete cessation of menstrual flow. These changes can include hot flushes and other symptoms associated with menopause.
It is crucial for women facing cancer treatment, especially those going through menopause or pregnancy, to be aware that the effects of chemotherapy on fertility, including sperm production in males and females, can differ based on several factors such as age and type of treatment received. Younger women generally have a higher chance of regaining their fertility post-treatment compared to older individuals. Some specific treatments may cause more significant damage to the ovaries or uterus than others.
To mitigate these potential issues, it is essential for women with ovarian cancer to explore options for preserving fertility before commencing radiation treatments. Techniques like freezing ovarian tissue or eggs offer hope for future conception when the time is right. By arming themselves with knowledge and seeking support from oncology professionals and support groups, women can navigate the emotional challenges associated with infertility during their battle against cancer and menopause.
In our upcoming blog posts, we will delve deeper into specific types of cancers that affect female fertility, including ovarian cancer and its impact on pregnancy. Stay tuned as we uncover valuable insights into this complex intersection between life, disease, and oncology in menopause.

Exploring the Relationship between Chemotherapy and Infertility
Chemotherapy, a commonly used oncology treatment during pregnancy, can have various effects on the body, including its potential impact on fertility. One significant concern for many individuals undergoing chemotherapy is its potential impact on fertility. Let’s delve into this topic to understand the relationship between chemotherapy and infertility, as well as its potential effects on menopause and radiation therapy.
Chemotherapy Drugs and Reproductive Cell Damage
Chemotherapy drugs in oncology are designed to target and destroy rapidly dividing cells, such as cancer cells. Unfortunately, these drugs can also affect healthy cells in the body, including reproductive cells and the ovaries. The damage caused by chemotherapy to these cells can lead to fertility problems in some cases, especially during pregnancy.
The extent of reproductive cell damage in testicular cancer patients depends on several factors, including the specific chemotherapy drugs used and their dosage. Some cancer treatments, such as alkylating agents like Cyclophosphamide, have a higher likelihood of causing infertility compared to other chemotherapy drugs.
Types of Cancer and Infertility Risks
In addition to the type of chemotherapy drug used, certain types of cancer, such as ovarian or testicular cancer, pose a higher risk of infertility due to radiation. The location or nature of the tumor can play a role in affecting fertility, especially when it develops near or within reproductive organs. For example, cancers that affect the ovaries or testicles may directly impact their function and lead to menopause.
It is important for individuals diagnosed with cancer to discuss their fertility concerns, including the potential impact of chemotherapy medicines, radiation therapy, and hormone therapy, with an oncologist before starting treatment. Understanding individual risks based on the type and stage of cancer will help patients make informed decisions regarding their future family planning options, considering the potential effects of chemo drugs.
Importance of Early Discussions about Fertility Concerns
Discussing fertility concerns with a cancer doctor prior to starting cancer treatments, such as chemotherapy or cancer surgery, is crucial for patients diagnosed with testicular cancer. This allows individuals to understand how their specific treatment plan may impact their future chances of having children. By having this knowledge, patients can consider options like egg or sperm freezing before beginning therapy.
Moreover, early discussions about fertility concerns enable oncologists to tailor treatment plans accordingly. In some cases, alternative chemotherapy drugs or lower dosages may be recommended to minimize the impact on ovaries and radiation while still effectively treating the cancer. This can help reduce the risk of early menopause and the need for surgery.
Ongoing Research and Minimization of Impact
Research in the field of oncology continues to explore ways to minimize the impact of chemotherapy on fertility in testicular cancer patients. Various strategies, such as using protective agents, are being investigated by the cancer care team to shield reproductive cells from damage during treatment. These advancements aim to provide individuals with more options for preserving their fertility while undergoing cancer treatments like chemotherapy and radiation.
Staying informed about ongoing research and advancements in cancer treatments, including hormone therapy for menopause and testicular cancer, is essential. By keeping up-to-date with the latest developments, patients can have meaningful discussions with their healthcare providers and make well-informed decisions regarding their fertility preservation options.
Fertility preservation options during cancer treatment
Women facing cancer treatment, including chemotherapy, radiation therapy, and hormone therapy, have various options for preserving their fertility, including egg freezing, embryo cryopreservation, and ovarian tissue freezing. These methods allow women to potentially have biological children after completing cancer treatment and going through menopause.
Preserving your fertility for the future
One concern that many women may have is the potential impact of hormone therapy on their fertility, especially for those undergoing cancer care for testicular cancer or prostate cancer. Fortunately, there are several fertility preservation options available that can help address this concern and provide hope for starting a family in the future.
Egg freezing
One popular method of fertility preservation for individuals undergoing testicular cancer treatment is egg freezing. This involves retrieving mature eggs from a woman’s ovaries and freezing them for later use. The process typically starts with hormone injections to stimulate the ovaries to produce multiple eggs. Once the eggs have reached maturity, they are collected through a minor surgical procedure known as egg retrieval, which can be done before cancer surgery, chemo, or radiation.
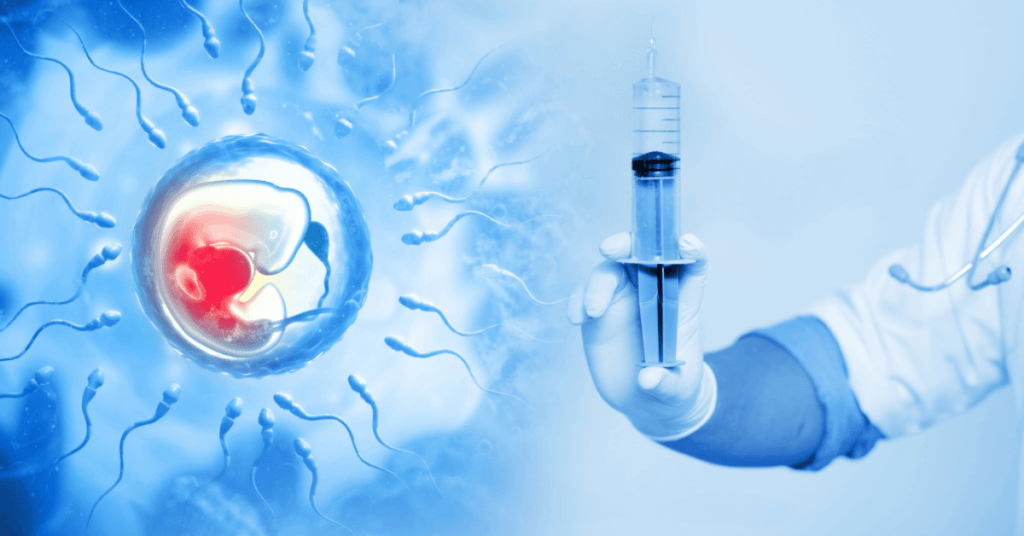
After retrieval, the eggs are carefully frozen using a technique called vitrification at a fertility clinic. This rapid freezing method helps prevent ice crystal formation, which can damage the delicate structure of the eggs. When the woman is ready to conceive in the future and seeks help from a fertility expert, the frozen eggs can be thawed and fertilized with sperm through in vitro fertilization (IVF) techniques before being transferred into her uterus to address fertility problems.
Embryo cryopreservation
Another option for fertility preservation in patients undergoing prostate cancer treatment, such as surgery, chemo, or radiation, is embryo cryopreservation. This method involves fertilizing retrieved eggs with sperm to create embryos before freezing them. The process is similar to IVF but instead of transferring fresh embryos into the woman’s uterus immediately, they are frozen for future use.
Embryo cryopreservation offers advantages for couples facing fertility problems. It allows those seeking fertility treatment at a fertility clinic to preserve their joint genetic material for future use when they are ready to start a family together. Frozen embryos have higher survival rates compared to frozen eggs, reducing fertility risks during thawing and transfer procedures.
Ovarian tissue freezing
For women who cannot undergo traditional fertility preservation methods such as surgery, chemotherapy, or radiation due to certain medical conditions or time constraints, ovarian tissue freezing may be a viable option. This procedure involves surgically removing a piece of the woman’s ovary, which contains immature eggs, and freezing it for later use. This method is particularly relevant for women with prostate cancer.
Ovarian tissue freezing, an experimental procedure, has shown promising results in recent years for women facing fertility problems due to cancer treatment. The frozen tissue can be thawed and transplanted back into the body after surgery, chemo, or radiation. Once transplanted, the tissue can potentially resume its normal function, allowing natural conception.
Timing is crucial
Fertility preservation procedures for women should ideally be done before starting chemotherapy or radiation therapy. These treatments can have detrimental effects on a woman’s reproductive system and may cause irreversible damage to eggs or ovarian function. Therefore, it is essential to consult with a reproductive specialist as early as possible to discuss available options and create a personalized fertility preservation plan. This is especially important for women undergoing surgery or prostate treatment.
The timing of fertility preservation for prostate cancer patients depends on individual circumstances and the schedules of chemo, radiation, and surgery treatments. In some cases, it may be necessary to slightly delay cancer treatment to complete fertility preservation procedures. This decision should be made in collaboration with oncologists and reproductive specialists to optimize cancer treatment and future fertility outcomes.
Financial assistance programs
It is important to note that fertility preservation procedures, such as chemo and surgery, can be costly. However, financial assistance programs are available that may help cover some or all of the associated expenses. Some insurance plans provide coverage for fertility treatments, including those related to cancer treatment-induced infertility.
Various nonprofit organizations offer grants and financial aid specifically aimed at supporting individuals seeking fertility preservation during chemo and surgery. These programs aim to reduce financial barriers and make these vital services more accessible.

Risks and Challenges of Chemotherapy-Induced Infertility
Chemotherapy treatment can have a significant impact on a woman’s fertility, leading to various risks and challenges that can cause emotional distress and uncertainty. Let’s delve into some of the key concerns associated with chemotherapy-induced infertility, including the potential need for surgery.
Emotional Distress and Feelings of Loss
Infertility caused by chemotherapy can be an incredibly difficult experience for many women. The inability to conceive a child naturally may evoke profound emotions such as sadness, grief, and a sense of loss. It is crucial to acknowledge these feelings and seek support from loved ones, healthcare professionals, or support groups who understand the unique challenges faced by individuals in this situation.
The desire to have children is deeply ingrained in many individuals, so when faced with the possibility of not being able to conceive due to chemotherapy treatment, it can be devastating. Coping with these emotions requires resilience and self-care. Engaging in activities that bring joy, seeking therapy or counseling services, or joining infertility support groups can provide solace during this trying time.
Uncertainty Surrounding Future Fertility Outcomes
One of the most challenging aspects of chemotherapy-induced infertility is the uncertainty surrounding future fertility outcomes. Each person’s response to treatment varies, making it difficult to predict whether fertility will be affected permanently or temporarily. This uncertainty adds an additional layer of stress during an already challenging period.
It is essential for individuals undergoing chemotherapy to have open discussions with their healthcare providers about potential fertility risks associated with specific treatments. This allows them to make informed decisions about their reproductive options before starting treatment. Understanding the potential impact on fertility can help alleviate anxiety and empower individuals to take proactive steps towards preserving their future fertility if desired.
Regret Over Missed Fertility Preservation Opportunities
In some cases, individuals may experience regret if they did not pursue fertility preservation options before starting chemotherapy treatment. Fertility preservation techniques such as egg freezing or embryo cryopreservation can provide a glimmer of hope for future family planning. However, these options need to be explored and pursued before treatment begins.
It is important for healthcare professionals to discuss fertility preservation options with patients before initiating chemotherapy. This proactive approach ensures that individuals are aware of the potential risks and have the opportunity to make decisions based on their personal circumstances and desires. Having this information beforehand can help prevent regret later on.
Coping with Long-Term Impacts on Relationships and Family Planning
Chemotherapy-induced infertility can have long-term impacts on relationships and family planning. The inability to conceive naturally may strain intimate partnerships, leading to feelings of frustration, guilt, or blame. Open communication between partners is crucial during this time, as it allows for mutual support and understanding.
Family planning may also require alternative paths such as adoption or assisted reproductive technologies like in vitro fertilization (IVF). These options come with their own set of challenges, including financial considerations and emotional stress. It is essential for couples to explore all available avenues together while seeking guidance from healthcare professionals specializing in fertility issues.
Seeking Support from Healthcare Professionals and Counselors
Navigating the challenges associated with chemotherapy-induced infertility requires a strong support system. Healthcare professionals who specialize in reproductive medicine can provide valuable guidance throughout the process. They can offer insights into fertility preservation techniques or refer individuals to appropriate specialists who can address their unique needs.
Counselors or therapists who specialize in infertility-related concerns can also play a vital role in helping individuals cope with the emotional impact of chemotherapy-induced infertility. These professionals provide a safe space for individuals to express their emotions, work through grief, and develop coping strategies.
Support groups consisting of individuals going through similar experiences with ed and fertility treatment offer an additional layer of comfort and understanding. Sharing stories, exchanging advice, and receiving encouragement from others facing similar challenges with ed and fertility treatment can be immensely beneficial during this journey.

Effects of chemotherapy on female fertility
Chemotherapy drugs can have a significant impact on female fertility, particularly by affecting the eggs in the ovaries. This can lead to a decrease in ovarian reserve, which refers to the number and quality of eggs available for fertilization. The extent of this impact varies depending on several factors, including age, type of chemotherapy drug used, and dosage administered.
One of the potential effects of chemotherapy on female fertility is the temporary or permanent cessation of menstruation during treatment. This occurs because chemotherapy drugs can disrupt the normal hormonal balance required for regular menstrual cycles. For some women, their periods may return after completing treatment, while others may experience long-term or even permanent changes in their menstrual patterns.
The risk of early menopause is higher for women who undergo fertility treatment. Menopause typically occurs naturally in women around their late 40s or early 50s when the ovaries stop producing eggs and hormones like estrogen and progesterone. However, chemotherapy can accelerate this process, leading to early menopause in some cases. Women who experience early menopause due to fertility treatment may face challenges when trying to conceive later in life.
Regular monitoring of hormone levels and ovarian function is crucial for gaining insights into potential fertility issues caused by chemotherapy. By tracking these parameters throughout treatment and beyond, healthcare professionals can identify any signs of ovarian failure or diminished ovarian reserve. Early detection allows for timely intervention and appropriate counseling regarding alternative options such as egg freezing or assisted reproductive technologies.
Impact of chemotherapy on male fertility
Chemotherapy can have a significant impact on male fertility, affecting both sperm production and quality. The drugs used in chemotherapy can cause damage to the testicles, where sperm cells are produced. This damage can lead to a decrease in the number and quality of sperm, making it more difficult for men to conceive.
The severity of infertility can vary depending on the specific drugs used in chemotherapy and individual factors. Some men may experience temporary changes in their sperm count or motility, while others may face permanent infertility. It is important to note that not all chemotherapy drugs have the same effect on fertility, and the degree of impact can differ from person to person.
One option for preserving male fertility before starting cancer treatment is sperm banking. Sperm banking allows men to store their sperm for future use if they wish to father children after completing chemotherapy. This process involves collecting ed semen samples and freezing them for later use. By banking their ed sperm before undergoing treatment, men can increase their chances of having biological children in the future.
In addition to potential long-term effects on fertility, some men may also experience temporary changes in their reproductive health during chemotherapy. These changes could include a decrease in sperm count or motility, which may affect their ability to conceive during treatment. However, it’s important to remember that these effects are not experienced by all men undergoing chemotherapy.
If you have concerns about male infertility as a result of chemotherapy, it is crucial to discuss them with your healthcare provider. They will be able to provide you with information about available options for ed and help guide you through the decision-making process. Your healthcare provider may refer you to a fertility specialist who can offer further guidance specific to your situation.
To summarize:
- Chemotherapy can damage sperm production and quality.
- The severity of infertility varies depending on the drugs used and individual factors.
- Sperm banking before treatment is an option for preserving fertility.
- Men may experience temporary or permanent changes in sperm count or motility.
- Discussing concerns with a healthcare provider is important for exploring available options.

Hormonal therapy for preserving fertility during chemotherapy
Chemotherapy drugs can have a significant impact on a person’s reproductive system, potentially leading to infertility. However, there are certain hormonal therapies available that can help protect the ovaries from the damaging effects of chemotherapy and increase the chances of preserving fertility.
One commonly used hormonal therapy is Gonadotropin-releasing hormone (GnRH) analogs. These medications work by suppressing ovarian function during chemotherapy treatment. By reducing the activity of the ovaries, GnRH analogs aim to minimize the risk of premature ovarian failure caused by chemotherapy drugs.
It is crucial to discuss the potential benefits and risks of hormonal therapy with an oncologist or reproductive specialist before starting treatment. Each individual may respond differently to these therapies, so regular monitoring is necessary to ensure their effectiveness.
Using hormone therapies alongside targeted therapy or other chemo drugs can provide additional protection for fertility. These treatments work together to minimize damage to the reproductive system while still targeting cancer cells effectively.
In addition to hormonal therapy, birth control methods may also be considered as part of fertility preservation during chemotherapy. Birth control pills can help regulate hormone levels and prevent unwanted pregnancies during treatment. It’s important to consult with a healthcare professional about suitable birth control options that align with individual circumstances.
One potential long-term effect of undergoing chemotherapy is early menopause. However, through careful consideration and appropriate use of hormone therapies, it may be possible to delay or mitigate this onset.
Coping with the Emotional Toll of Infertility After Chemotherapy
Infertility resulting from cancer treatment can be a devastating blow, both physically and emotionally. The impact it has on individuals and couples cannot be underestimated. The journey to parenthood is often filled with joy and anticipation, but when faced with the reality of infertility post-chemotherapy, it is natural to experience a range of intense emotions.
Grief, sadness, anger, and frustration are common feelings that arise when confronted with the inability to conceive after undergoing chemotherapy. It is important to acknowledge and validate these emotions rather than suppress them. Allow yourself the space to mourn the loss of your fertility while also recognizing that it is normal to feel this way.
One way to cope with the emotional toll of infertility is by seeking support from therapists who specialize in reproductive health or joining support groups. These professionals can provide guidance and understanding as you navigate through this challenging time. They can help you process your emotions, develop coping strategies, and offer valuable insights into managing the rollercoaster ride of infertility.
In addition to professional support, open communication with your partner and loved ones is crucial. Sharing your thoughts, fears, and frustrations can foster understanding within your relationships while providing much-needed emotional support. Your loved ones may not fully comprehend what you are going through, but their empathy can go a long way in alleviating some of the burden.
Exploring alternative family-building options can also bring a sense of hope amidst the challenges of infertility. Adoption or surrogacy are viable paths that many individuals choose after chemotherapy-induced infertility. While they may not replace biological parenthood entirely, they offer an opportunity for creating a loving family environment.
Adoption allows you to provide a nurturing home for a child in need while experiencing the joys of parenthood. Surrogacy enables you to have a biological connection by using another woman’s uterus to carry your child. Both options come with their own unique set of considerations, but they can provide a fulfilling and loving family dynamic.
Managing the physical symptoms that often accompany infertility, such as hot flushes, is also essential for emotional well-being. Taking steps to alleviate discomfort through symptom management techniques can help you regain a sense of control over your body. This may involve lifestyle changes, medication, or alternative therapies. Consult with your healthcare provider to explore the options available to you.
While nerves and uncertainty may be constant companions during this journey, it is crucial to remember that infertility does not define your worth or happiness. It is an obstacle that you can overcome with resilience and support. Surround yourself with positive influences and engage in activities that bring you joy and fulfillment.

Alternative methods for fertility preservation during cancer treatment
Experimental techniques like ovarian tissue cryopreservation and in vitro maturation offer additional options for fertility preservation.
There are alternative methods that can be explored. One such method is ovarian tissue cryopreservation, which involves removing a small piece of the ovary and freezing it for future use. This technique allows women to potentially regain their fertility after completing cancer treatment. However, it’s important to note that ovarian tissue cryopreservation is still considered experimental and may not be widely available or successful in all cases.
Another experimental technique is in vitro maturation (IVM), which involves retrieving immature eggs from the ovaries and allowing them to mature in a laboratory setting before being frozen. This approach offers hope for women who cannot undergo traditional IVF due to time constraints or medical reasons. However, similar to ovarian tissue cryopreservation, IVM is still being researched and its success rates may vary.
Discussing the potential benefits, risks, and success rates with a reproductive specialist is crucial when considering alternative methods.
It’s essential for individuals considering alternative methods of fertility preservation during cancer treatment to have open discussions with reproductive specialists. These specialists can provide valuable insights into the potential benefits, risks, and success rates associated with different approaches.
By consulting with a reproductive specialist, patients can gain a better understanding of how these experimental techniques work and whether they are suitable for their unique circumstances. The specialist can also provide information on any ongoing clinical trials or advancements in the field that could enhance the chances of successful fertility preservation.
Ovarian suppression using hormonal therapies during chemotherapy may also be an option to protect fertility.
In addition to experimental techniques like ovarian tissue cryopreservation and IVM, there is another option known as ovarian suppression using hormonal therapies. This approach aims to protect fertility by temporarily shutting down the ovaries during chemotherapy treatment.
Hormonal therapies, such as GnRH agonists, can be administered prior to and during chemotherapy to reduce the impact of the treatment on the ovaries. By suppressing ovarian function, these therapies may help preserve a woman’s fertility. However, it’s important to note that the effectiveness of this method can vary depending on individual factors and the specific cancer treatment being received.
Each individual’s unique circumstances should be considered when exploring alternative fertility preservation approaches.
There is no one-size-fits-all approach. It is crucial to consider each individual’s unique circumstances when exploring alternative methods.
Factors such as age, type of cancer, stage of cancer, and treatment plan all play a role in determining which fertility preservation options are most suitable. For example, some individuals may have limited time for fertility procedures due to the urgency of their cancer treatment, while others may have specific medical considerations that limit their choices.
By consulting with healthcare professionals specializing in reproductive health and oncology, individuals can receive personalized guidance based on their specific situation. These experts can assess the feasibility and potential success rates of different approaches and help patients make informed decisions about their fertility preservation options.
Long-term effects of chemotherapy on reproductive health
Chemotherapy is a crucial treatment option for many cancer patients, but it can have lasting impacts on reproductive health that go beyond the immediate concern of infertility. It’s important to understand these potential long-term effects in order to make informed decisions about family planning post-treatment.
Pregnancy complications and risks
Women who become pregnant after undergoing cancer treatment may face a higher risk of complications compared to those who haven’t had chemotherapy. These complications can include preterm birth or low birth weight, which can pose challenges for both the mother and the baby. It is essential for healthcare professionals to closely monitor pregnancies in cancer survivors to ensure early detection of any potential issues.
Increased risk of gynecological conditions
Certain chemotherapy drugs have been associated with an increased risk of developing gynecological conditions later in life. These conditions can range from hormonal imbalances and menopause symptoms to more serious issues such as damage to reproductive organs. Regular check-ups with healthcare providers are crucial for detecting any signs or symptoms of these conditions early on, allowing for timely intervention if necessary.
Importance of regular monitoring
Regular monitoring by healthcare professionals is vital for individuals who have undergone chemotherapy, as it enables the detection and management of any long-term effects on reproductive health. This includes keeping track of hormone levels, assessing the overall functioning of the reproductive system, and identifying any abnormalities or changes that may require further investigation or treatment.
Informed decision-making about family planning
Understanding the potential risks associated with chemotherapy is key when making decisions about family planning after cancer treatment. Being aware of the possible long-term effects allows individuals to weigh their options and explore alternative paths if necessary. This may involve considering fertility preservation techniques before starting treatment or exploring adoption or surrogacy as alternatives to biological parenthood.
It’s important to remember that while some individuals may experience permanent infertility after chemotherapy, others may still be able to conceive naturally. Each person’s situation is unique, and it’s crucial to have open and honest discussions with healthcare providers to fully understand the potential impact on reproductive health.
Overcoming Infertility Challenges Post-Chemotherapy
Chemotherapy is a vital treatment option for many individuals battling cancer. However, one of the concerns that often arise is whether chemotherapy can make you infertile. The good news is that there are ways to overcome infertility challenges after undergoing chemotherapy.
Assisted Reproductive Technologies: A Ray of Hope
Assisted reproductive technologies (ART), such as in vitro fertilization (IVF), have revolutionized the field of reproductive medicine. IVF involves fertilizing eggs with sperm outside the body and then transferring the resulting embryo into the uterus. This technique has provided hope to countless couples facing infertility issues post-chemotherapy.
For individuals who have undergone chemotherapy and are concerned about their fertility prospects, consulting with a fertility specialist is crucial. These experts possess specialized knowledge and experience in navigating infertility challenges after cancer treatment. They can provide personalized insights into available options based on individual circumstances, ensuring that each person receives tailored guidance.
Exploring Alternative Routes: Donor Eggs or Sperm
In some cases, natural conception may not be possible due to chemotherapy-induced infertility. However, this does not mean that parenthood is out of reach. Many individuals turn to alternative routes such as using donor eggs or sperm to achieve pregnancy.
Donor eggs can be obtained from women who are willing to contribute their healthy eggs for assisted reproduction purposes. Similarly, donor sperm can be used when male partners face fertility problems due to chemotherapy treatments. These options allow individuals to experience the joys of parenthood despite the challenges they have faced.
Nurturing Psychological Support: A Crucial Component
Embarking on a journey towards parenthood after chemotherapy-induced infertility can be emotionally challenging. It is essential to recognize and address these psychological aspects throughout the process. Seeking psychological support from therapists or support groups specializing in infertility can provide individuals with the necessary tools to cope with the ups and downs of assisted reproduction techniques.
Dealing with infertility challenges can evoke a range of emotions, including sadness, frustration, and anxiety. Having a support system in place helps individuals navigate these feelings and find strength during difficult times. Remember, you are not alone in this journey, and seeking support is a sign of resilience and self-care.
Holding onto Hope: The Key to Overcoming Challenges
When faced with fertility obstacles after chemotherapy, it is easy to feel disheartened. However, it is crucial to remain hopeful and open-minded throughout the process. There are various paths to parenthood that can be explored, each offering its unique set of possibilities.
Consider immunotherapy drugs as an example. These innovative treatments have shown promising results in preserving fertility for some cancer patients undergoing chemotherapy. By exploring all available options and staying positive, individuals can increase their chances of overcoming infertility challenges.

Conclusion: Empowering cancer patients through knowledge about fertility preservation
Empowering cancer patients with knowledge about fertility preservation is crucial in helping them make informed decisions about their reproductive health. Understanding the relationship between chemotherapy and infertility, exploring available options for fertility preservation during cancer treatment, and being aware of the risks and challenges associated with chemotherapy-induced infertility are key aspects that can significantly impact a patient’s fertility journey.
Chemotherapy can have varying effects on both female and male fertility. While it may cause temporary or permanent damage to reproductive organs, there are several methods available to preserve fertility during treatment. Hormonal therapy is one such option that can help protect eggs in females and sperm in males from the damaging effects of chemotherapy.
Coping with the emotional toll of infertility after chemotherapy is an important aspect that should not be overlooked. The psychological impact of facing infertility can be overwhelming, and providing support and resources to patients navigating this journey is essential.
In addition to traditional methods, alternative approaches for fertility preservation during cancer treatment are emerging. These include experimental techniques like ovarian tissue cryopreservation or testicular tissue freezing, which offer hope for future reproductive possibilities.
Understanding the long-term effects of chemotherapy on reproductive health is also crucial. It allows patients to plan ahead and make informed decisions about family-building options post-treatment.
While overcoming infertility challenges after chemotherapy may seem daunting, it’s important to remember that there are various assisted reproductive technologies available today that can help individuals achieve their dreams of parenthood. Seeking guidance from healthcare professionals specializing in fertility can provide valuable insights into personalized treatment options.
By empowering cancer patients with knowledge about fertility preservation, we aim to alleviate some of the uncertainties surrounding this topic. It is our mission to ensure that individuals facing cancer treatments have access to accurate information so they can make well-informed choices regarding their reproductive future.
Remember, you are not alone in this journey. Reach out to your healthcare provider or a specialized fertility clinic who can guide you through the process and provide the support you need.
FAQs:
Q: Can chemotherapy always make a person infertile?
A: While chemotherapy can have detrimental effects on fertility, it does not always result in infertility. The impact of chemotherapy on fertility varies depending on factors such as the type and dosage of drugs used, age, and individual response to treatment.
Q: Is fertility preservation during cancer treatment expensive?
A: The cost of fertility preservation can vary depending on the chosen method. Some options, like sperm or embryo freezing, may be more affordable compared to experimental techniques such as ovarian tissue cryopreservation. It is advisable to consult with your healthcare provider and insurance company to understand the financial implications.
Q: Are there any support groups or resources available for individuals facing infertility after chemotherapy?
A: Yes, there are numerous support groups and resources available for individuals navigating infertility post-chemotherapy. These platforms offer emotional support, information sharing, and guidance from others who have gone through similar experiences. Connecting with these communities can provide valuable insights and help ease the emotional burden.
Q: Can hormonal therapy completely protect fertility during chemotherapy?
A: Hormonal therapy can help protect eggs in females and sperm in males from the damaging effects of chemotherapy. However, its effectiveness may vary depending on individual circumstances. It is essential to consult with a reproductive specialist who can evaluate your specific situation and recommend suitable options.
Q: Are there any lifestyle changes that can improve fertility after chemotherapy?
A: Adopting a healthy lifestyle that includes regular exercise, a balanced diet, stress management techniques, and avoiding harmful substances like tobacco or excessive alcohol consumption may positively impact overall reproductive health post-chemotherapy. However, it is important to note that individual responses may vary, so consulting with a healthcare professional is recommended for personalized advice.




