
Have you ever heard of azoospermia? It’s a medical condition that affects men and can have a significant impact on their fertility. Azoospermia is when a man produces no sperm or very little sperm, making it challenging for them to father children. For male infertility patients, severe oligozoospermia, asthenozoospermia, and teratozoospermia can also contribute to difficulties in conception.
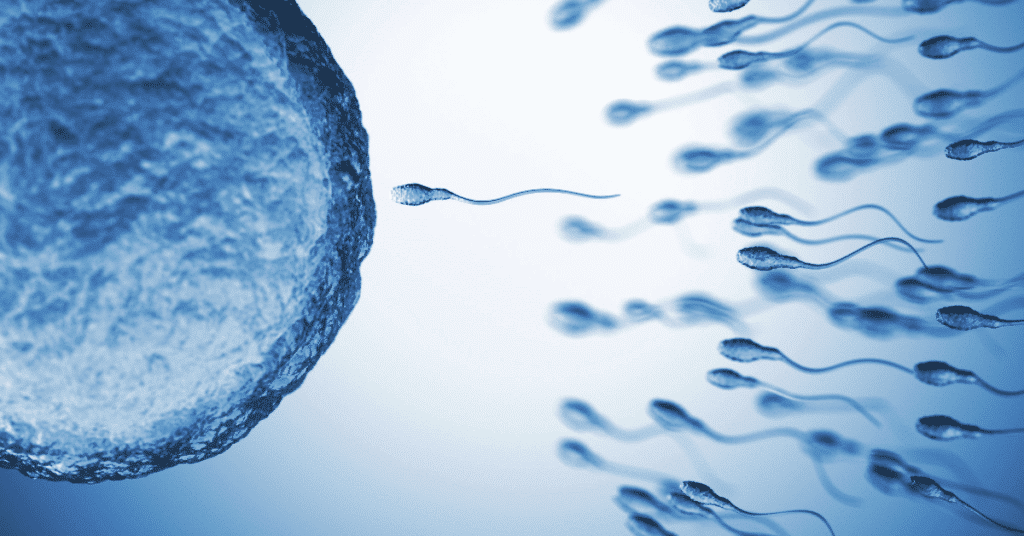
The first step in diagnosing male infertility patients is through a semen analysis. This involves examining a sample of semen under a microscope to determine the number and quality of sperm present, including asthenozoospermia, teratozoospermia, and severe oligozoospermia. If there are no sperm found, then the diagnosis of azoospermia is made.
Amino acids are crucial for male fertility and sperm production, and they can be found in a variety of foods such as eggs, meat, and dairy products. Ensuring that your diet includes these amino acids may help improve your chances of producing healthy sperm, especially for those who suffer from male infertility or testicular azoospermia, which is the absence of sperm in semen for azoospermic men.
There are several factors that can cause male infertility, including hormonal imbalances, genetic disorders, infections, and certain medications. Azoospermia and asthenozoospermia are common conditions that affect azoospermic men, leading to the absence of sperm or low sperm motility. Teratozoospermia is another condition that affects sperm morphology and can contribute to male infertility. Congenital azoospermia is when a man is born without the ability to produce sperm.
Treatment options for male infertility, including azoospermia, severe oligozoospermia, and asthenozoospermia, depend on the underlying cause. Hormone therapy may be used if there is an imbalance in hormone levels. Surgery may be necessary if there is an obstruction preventing the flow of sperm. Assisted reproductive technologies such as IVF or ICSI may also be used to help couples conceive and improve male fertility.
In some cases, lifestyle changes such as quitting smoking or reducing alcohol intake may also help improve fertility outcomes for men with male infertility, severe oligozoospermia, abnormal semen, and impaired spermatogenesis.
Male Reproductive System: Understanding the Anatomy
Parts of the Male Reproductive System
The male reproductive system is composed of several organs that work together to produce, store, and transport sperm. These organs include the testis, which produces testosterone – a hormone responsible for the development of secondary sexual characteristics. Testicular azoospermia is a condition that affects some infertile men by preventing the production of sperm in the testes.
- Testicles (or testes): The two oval-shaped glands located in the scrotum that produce and store sperm, as well as testosterone, which is a hormone responsible for male characteristics. In some cases, testicular azoospermia can occur, which is the absence of sperm in the semen due to a blockage in the ejaculatory duct. This condition can lead to male infertility.
- Epididymis: A long, coiled tube attached to each testicle where sperm mature and are stored. It is connected to the ejaculatory duct which transports sperm out of the body. Testicular azoospermia, a condition where the testicles do not produce sperm, can cause male infertility. Varicoceles, enlarged veins in the scrotum, may also affect sperm production in the epididymis.
- Vas deferens: A muscular tube that carries mature sperm from the epididymis to the ejaculatory ducts during ejaculation. Varicoceles, a common cause of male infertility, can affect the function of the vas deferens and lead to testicular azoospermia, a type of male factor infertility.
- Seminal vesicles: Glands located behind the bladder that produce a fluid rich in fructose and other nutrients that help nourish and protect sperm. This fluid is carried through the ejaculatory duct, which can be affected by varicoceles, a common cause of male infertility. In some cases, testicular azoospermia may also be a factor.
- Prostate gland: A walnut-sized gland located below the bladder that produces an alkaline fluid, containing testosterone, that helps neutralize acidic vaginal secretions and enhance sperm motility. Testicular azoospermia, a condition that causes male infertility due to low levels of FSH, can also affect the prostate gland.
- Urethra: The tube running through the penis that carries semen and urine out of the body during ejaculation. Testosterone plays a crucial role in sperm quality, and low levels of testosterone can lead to male infertility. In some cases, testicular azoospermia can also contribute to infertility by preventing sperm from being present in semen.
Testicular Tissue and Sperm Production
The testicle is the primary site of spermatogenesis—the process of producing mature sperm cells, and is also closely associated with male infertility. It consists of tiny coiled tubes called seminiferous tubules where immature germ cells develop into mature sperm cells. Testicular azoospermia, a condition where no sperm is present in the semen, is a common cause of infertility in men. This condition is often linked to low levels of testosterone, which can also contribute to infertility in infertile men.
Testosterone, a hormone produced by specialized cells within the testicular tissue called Leydig cells, plays a crucial role in male fertility. It regulates secondary sex characteristics such as facial hair growth, muscle mass development, and deepening of voice, but it also stimulates spermatogenesis. The production of testosterone is regulated by luteinizing hormone (LH) and follicle-stimulating hormone (FSH). In addition, testosterone can be used in in vitro fertilization techniques such as intracytoplasmic sperm injection (ICSI). However, high levels of testosterone can interfere with pregnancy.
Scrotal ultrasonography is a common diagnostic tool used to assess testicular size, volume, abnormalities or masses in males with infertility issues. This imaging technique can detect varicoceles (enlarged veins in the scrotum), tumors or cysts on or around testicles. It is also useful in evaluating successful sperm retrieval, sperm counts, and sperm quality in cases of low sperm count.
Ejaculatory Ducts and Sperm Transport
During ejaculation, sperm travel through the vas deferens to the ejaculatory ducts, which are responsible for transporting sperm from the testicles to the urethra. In cases of testicular azoospermia, where there is no sperm present in the semen due to male infertility, testosterone and FSH hormone levels may be affected. The seminal vesicles and prostate gland produce fluids that mix with the sperm in the ejaculatory ducts to form semen.
Undescended testicles, or cryptorchidism, is a common congenital condition where one or both testicles fail to descend into the scrotum. This can lead to decreased testicular volumes and affect spermatogenesis, leading to male factor infertility in patients. In some cases, surgery may be necessary to correct this condition and improve testosterone levels and increase the chances of pregnancy for infertile men.
Types of Azoospermia: Exploring the Differences
Obstructive Azoospermia: When a Blockage Occurs in the Reproductive Tract
Obstructive azoospermia is one of the two types of azoospermia, a condition that causes male infertility in which infertile men are unable to produce sperm. It occurs when there is a blockage in the reproductive tract preventing sperm from being ejaculated. The blockage can occur anywhere along the reproductive tract, including the epididymis, vas deferens, or ejaculatory ducts. Testosterone levels may be affected by this condition, and it can make it difficult for couples to achieve pregnancy.
There are many causes of obstructive azoospermia, a type of male infertility, such as previous surgeries, infections, or congenital abnormalities. In some cases, patients may not even realize they have this condition until they try to conceive with their partner and fail. Testosterone levels may also be affected in men with obstructive azoospermia.
If you suspect that you have obstructive azoospermia, it’s essential for patients to see a doctor who specializes in male infertility and testosterone. They will perform a thorough evaluation to determine the cause of your condition and recommend an appropriate treatment plan.
Some common treatments for male infertility due to obstructive azoospermia include surgery to remove any blockages or bypass them entirely. In other cases, doctors may recommend assisted reproductive technologies (ART) such as intrauterine insemination (IUI) or in vitro fertilization (IVF). Testosterone therapy may also be an option for some patients.

Non-Obstructive Azoospermia: When There is a Problem with Sperm Production
Non-obstructive azoospermia, which affects approximately 1% of all men, is a condition where there is a problem with sperm production. This type of azoospermia accounts for up to 20% of male infertility cases. Patients with non-obstructive azoospermia may have low levels of testosterone.
There are many reasons why non-obstructive azoospermia, a common cause of male infertility, occurs, including hormonal imbalances such as low testosterone levels, genetic defects, chemotherapy treatments for cancer, or environmental factors such as exposure to toxins.
There are several options available for male infertility. In cases of testicular azoospermia, doctors may prescribe testosterone to help stimulate sperm production. Alternatively, they may recommend ART such as IUI or IVF.
In some cases of male infertility, men with non-obstructive azoospermia may be able to father children through a procedure called testicular sperm extraction (TESE). During this procedure, a surgeon removes small samples of testicular tissue and extracts any viable sperm for use in assisted reproductive technology (ART). Testosterone levels may also be evaluated to determine if they are contributing to the infertility.
Abnormal Sperm and Chromosomal Defects
Abnormal sperm and chromosomal defects are common causes of both obstructive and non-obstructive azoospermia, leading to infertility in men. These conditions can result in low sperm count or no sperm production, which may require testosterone treatment to improve fertility.
Some common types of abnormal sperm include:
- Asthenozoospermia: When the sperm cannot swim properly.
- Teratozoospermia: When the shape of the sperm is abnormal.
- Oligozoospermia: When there is a low number of sperm present in semen, which can be a symptom of male infertility. Testicular azoospermia, the absence of sperm in semen due to testicular dysfunction, can also contribute to male infertility. In some cases, low testosterone levels may also be a factor.
Chromosomal defects can also cause azoospermia in infertile men by disrupting normal spermatogenesis and leading to male infertility. Some common chromosomal abnormalities that can lead to azoospermia and low testosterone levels include Klinefelter syndrome, Turner syndrome, or Y-chromosome deletions.
Causes of Azoospermia: Understanding the Underlying Factors
Testicular Causes
One of the leading causes of male infertility is testicular factors such as injury, infection, or surgery. These factors can interfere with sperm production and transport. Injury to the testicles can occur due to accidents or sports-related injuries. Infections such as mumps orchitis can cause inflammation in the testicles leading to damage and reduced sperm production. Surgery in the pelvic area, including prostate surgery, may also affect sperm production by damaging the tubes that carry semen.
Male Factor Infertility
Male factor infertility is a common cause of azoospermia and can be due to problems with sperm production or transport. Sperm production issues occur when there is a problem with germ cells’ formation, which leads to an inadequate number of mature sperm cells produced. Transport issues arise when there is a blockage in the ducts that carry semen from the testes out through the penis during ejaculation.
Genetic Abnormalities
Genetic abnormalities are a factor in some cases of azoospermia, including Klinefelter syndrome and Y chromosome microdeletions. Klinefelter syndrome occurs when males have an extra X chromosome resulting in abnormal development of male sexual characteristics and infertility. Y chromosome microdeletions are missing pieces of genetic material on the Y chromosome that lead to low sperm count or no sperm at all.
Disorders and Diseases
Certain disorders and diseases can cause male infertility, such as cystic fibrosis, sickle cell anemia, and diabetes. Cystic fibrosis affects various organs in the body, including reproductive organs like vas deferens leading to blocked ducts that prevent sperms from reaching semen during ejaculation. Sickle cell anemia causes red blood cells to become rigid and sticky blocking blood flow throughout your body’s tissues causing damage to organs including testicles. Diabetes can cause damage to nerves, blood vessels, and muscles that control ejaculation.
Unknown Causes
In some cases, the cause of azoospermia may be unknown. However, it is essential to undergo testing to rule out any underlying issues. A comprehensive evaluation by a urologist or male infertility specialist can help determine if there are any reversible causes such as hormonal imbalances or infections that can be treated.
Identifying the Cause
Identifying the cause of azoospermia is crucial in determining the appropriate treatment options for male infertility. Treatment options depend on the underlying cause of azoospermia and include surgical interventions, hormone therapy, and assisted reproductive techniques such as intracytoplasmic sperm injection (ICSI) or testicular sperm extraction (TESE).

Azoospermia Diagnosis: Tests and Diagnosis Methods
Semen Analysis: The First Step in Diagnosing Azoospermia
Semen analysis is the first step in diagnosing male infertility and azoospermia. This test evaluates various sperm parameters such as sperm count, motility, morphology, volume, and pH level. If the semen analysis report shows no sperm presence in the sample, it indicates male infertility and azoospermia.
Apart from azoospermia, semen analysis also helps diagnose other abnormal semen conditions such as asthenozoospermia (low sperm motility) and teratozoospermia (abnormal sperm morphology), which are common causes of male infertility. Semen analysis can be performed at a fertility clinic or a laboratory that specializes in reproductive health.
Testicular Biopsy: An Invasive Procedure to Diagnose Azoospermia
Testicular biopsy is an invasive procedure used to diagnose the underlying cause of male infertility, specifically azoospermia. This procedure involves removing a small piece of tissue from the testes for examination under a microscope. Testicular biopsy is usually recommended when there are no sperm present in the ejaculate or when obstructive azoospermia has been ruled out.
There are two types of testicular biopsy procedures – needle biopsy and open biopsy. Needle biopsy is less invasive than open biopsy but may not provide enough tissue samples for accurate diagnosis of male infertility and successful sperm retrieval. Open biopsy involves making a small incision on the scrotum to remove tissue samples directly from the testes, which can be useful in assessing sperm counts and sperm quality.
Ejaculatory Urinalysis: Non-Invasive Test to Determine Sperm Presence
Ejaculatory urinalysis is a non-invasive diagnostic test that can help determine if sperm are present in the semen or not, which is particularly useful in identifying testicular azoospermia, a major cause of male infertility. This test involves collecting urine immediately after ejaculation and examining it under a microscope for any signs of sperms.
Ejaculatory urinalysis is typically used when there are no sperms found during semen analysis, which can be an indication of male infertility. This test can help diagnose obstructive azoospermia, a condition where the sperm production is normal but blocked from reaching the semen.
Ultrasonography: Imaging Technique to Diagnose Azoospermia
Ultrasonography is an imaging technique that uses high-frequency sound waves to create images of the internal organs and tissues. This diagnostic method can be used to diagnose male infertility, azoospermia, and related syndromes by examining the reproductive system.
Transrectal ultrasonography (TRUS) is a type of ultrasonography that involves inserting a small probe into the rectum to examine the prostate gland and seminal vesicles for any abnormalities. This procedure can also be used for successful sperm retrieval in cases of male infertility and to evaluate sperm counts. Scrotal ultrasonography is another type of ultrasonic examination that evaluates testicular size, blood flow, and other structural abnormalities.
Genetic Testing: Identifying Genetic Causes of Azoospermia
Genetic testing is a diagnostic method used to identify genetic causes of azoospermia. Some genetic conditions such as Klinefelter syndrome, Y chromosome microdeletions, and cystic fibrosis gene mutations can cause azoospermia in males.
Genetic testing involves analyzing DNA samples obtained from blood or saliva samples. This test can help determine if there are any genetic mutations or chromosomal abnormalities that may be causing infertility in males, including those with testicular azoospermia or low sperm counts. In some cases, sperm retrieval may be necessary to obtain a sample for testing.
Thorough Physical Examination and Medical History Review
A thorough physical examination and medical history review are important steps in diagnosing male infertility, particularly azoospermia. During physical examination, the doctor will examine the genitals for any signs of abnormality such as undescended testes or varicocele.
Medical history review involves discussing personal medical history, family medical history, lifestyle factors, medication use, and exposure to environmental toxins that may affect fertility. For men, this may include a discussion of male infertility, sperm retrieval, sperm counts, and low sperm count.

How Common is Azoospermia? Exploring the Statistics
What is Azoospermia?
Azoospermia is a medical condition that affects men, characterized by the absence of sperm in their semen. It can be caused by either a problem with the testicles, which produce sperm, or an obstruction in the reproductive tract that prevents the sperm from being ejaculated. This condition is one of the leading causes of male infertility.
Infertility Cases and Sperm Counts
Infertility cases affect around 15% of couples worldwide, and male infertility accounts for about half of these cases. In men diagnosed with infertility, low sperm count or low semen volume are found in about 90% of them. However, azoospermia accounts for the remaining 10%.
The Prevalence of Azoospermia
Azoospermia is relatively rare compared to other male fertility issues. According to research studies, it affects approximately 1% of the male population. However, its prevalence varies depending on geographical location and ethnicity.
In addition to genetics and ethnicity, lifestyle factors such as smoking, alcohol consumption, drug abuse, and exposure to environmental toxins can also contribute to the development of male infertility, specifically azoospermia.
Sperm Retrieval Rates and Pregnancy Rates
Such as intracytoplasmic sperm injection (ICSI), sperm retrieval rates are generally lower for men with male infertility, low sperm count, or low semen volume.
However, despite lower retrieval rates for men with azoospermia compared to those with other types of infertility issues related to sperm counts or semen quality problems; pregnancy rates can still be achieved through ARTs like ICSI.
Understanding FSH Levels
Follicle-stimulating hormone (FSH) levels can be used by doctors to determine the underlying cause of male infertility, specifically azoospermia. Higher FSH levels indicate testicular failure, while lower levels suggest a blockage in the reproductive tract.
In cases of male infertility with obstructive azoospermia, surgical procedures such as vasectomy reversal or epididymal sperm aspiration can be used to retrieve sperm for ARTs. However, if the cause of male infertility is non-obstructive azoospermia, treatment options may include hormone therapy or testicular biopsy.

Pretesticular vs Posttesticular Azoospermia: What’s the Difference?
Azoospermia is a condition commonly associated with male infertility, where there is no sperm present in the semen. It can be caused by either pretesticular or posttesticular factors. Pretesticular azoospermia is caused by issues with hormone production, while posttesticular azoospermia is caused by problems with sperm transport or production.
Pretesticular Azoospermia
Pretesticular azoospermia, a common cause of male infertility, occurs when there are issues with hormone production that prevent the testicles from producing sperm. This type of azoospermia accounts for around 20% of all cases and can be caused by a variety of factors such as:
- Hypothalamic or pituitary disorders
- Anabolic steroid use
- Chemotherapy or radiation therapy
- Genetic conditions like Kallmann syndrome
Treatment options for male infertility and pretesticular azoospermia depend on the underlying cause. Hormone replacement therapy may be used to stimulate sperm production, while surgery may be necessary to correct any structural abnormalities.
Posttesticular Azoospermia
Posttesticular azoospermia, a common cause of male infertility, occurs when there are problems with sperm transport or production after it has left the testicles. This type of azoospermia accounts for around 80% of all cases and can be further divided into obstructive and non-obstructive subtypes.
Obstructive Posttesticular Azoospermia
Obstructive posttesticular azoospermia is a common cause of male infertility, occurring when there is a blockage preventing sperm from leaving the testes. This can occur due to:
- Congenital absence of vas deferens (CAVD)
- Infection or inflammation causing scarring
- Vasectomy
In these cases, surgical intervention may be necessary to remove the blockage and retrieve viable sperm for use in assisted reproductive technologies.
Non-Obstructive Posttesticular Azoospermia
Non-obstructive posttesticular azoospermia occurs when there is no sperm present in the semen due to a problem with sperm production. This can occur due to:
- Primary testicular failure
- Testicular cancer
- Testicular torsion or trauma
- Subclinical varicoceles
Subclinical varicoceles are a common cause of non-obstructive posttesticular azoospermia, where the veins in the scrotum become enlarged and disrupt blood flow to the testicles. This can lead to decreased sperm production and quality.
Treatment options for non-obstructive posttesticular azoospermia depend on the underlying cause. For example, testicular sperm extraction (TESE) is a surgical procedure that can be used to retrieve sperm from men with testicular azoospermia for use in assisted reproductive technologies.
Nonobstructive Azoospermia (NOA): Causes and Treatment Options
What is Nonobstructive Azoospermia?
Nonobstructive azoospermia (NOA) is a medical condition where there is no sperm present in the semen due to a problem with sperm production. This is different from obstructive azoospermia, where the sperm is produced but cannot be ejaculated due to a blockage. NOA accounts for approximately 10% of male infertility cases and can make it difficult or impossible for men to father children without intervention.
What Causes Nonobstructive Azoospermia?
There are several potential causes of nonobstructive azoospermia, including genetic factors, hormonal imbalances, testicular injury or infection, and certain medications or treatments. In some cases, the exact cause may be unknown.
Genetic factors can play a role in NOA, which can result in low sperm counts and require sperm retrieval. For example, Klinefelter syndrome, which occurs when males have an extra X chromosome (XXY instead of XY), can lead to impaired testicular function and ultimately, NOA. Other genetic conditions that may contribute to NOA include Y chromosome deletions and chromosomal translocations.
Hormonal imbalances can also cause NOA by interfering with the body’s ability to produce sperm. Conditions such as hypogonadism (low testosterone levels), hyperprolactinemia (high prolactin levels), and thyroid disorders can all impact fertility.
Testicular injury or infection can damage the tissue responsible for producing sperm and lead to NOA. Trauma to the testicles, exposure to toxins such as chemotherapy drugs or radiation therapy, and infections such as mumps orchitis are all potential causes of testicular damage.
Certain medications or treatments may also contribute to NOA. Chemotherapy drugs used in cancer treatment can damage the DNA within cells responsible for sperm production, while radiation therapy can damage the testicles and reduce sperm count. Some medications used to treat conditions such as depression or high blood pressure may interfere with sperm production.
What is Obstructive Azoospermia?
Obstructive azoospermia occurs when there is a blockage preventing the sperm from being ejaculated. Unlike NOA, men with obstructive azoospermia have normal sperm production but are unable to release it due to an obstruction in the reproductive tract.
There are several potential causes of obstructive azoospermia, including ejaculatory duct obstruction and vasal obstruction. Ejaculatory duct obstruction occurs when there is a blockage in one or both of the tubes that carry semen from the testicles to the urethra. Vasal obstruction occurs when there is a blockage in one or both of the vas deferens, which transport sperm from the testicles to the urethra.
How to Determine Obstructive Azoospermia
Determining whether a man has obstructive or nonobstructive azoospermia requires a thorough medical evaluation by a urologist or fertility specialist. The first step in diagnosing either condition typically involves analyzing semen samples for the presence of sperm.
If no sperm are present in the semen (azoospermia), further testing will be necessary to determine if there is an obstruction preventing ejaculation or if there is an issue with sperm production. This may involve hormone testing, genetic testing, ultrasound imaging, and other diagnostic tests.
Treatment Options for Nonobstructive Azoospermia
Treatment options for nonobstructive azoospermia depend on several factors, including the underlying cause of infertility and whether viable sperm can be retrieved for use in assisted reproductive technologies (ART).
In cases where viable sperm cannot be retrieved from semen samples, surgical sperm retrieval may be necessary to obtain sperm for use in ART. This may involve testicular sperm extraction (TESE), which involves removing a small piece of testicular tissue and extracting viable sperm, or percutaneous epididymal sperm aspiration (PESA), which involves using a needle to extract sperm from the epididymis.
Management and Treatment of Azoospermia: Available Options
Various Treatment Options for Azoospermia
Azoospermia is a condition that affects the ability to conceive, but there are various treatment options available. The treatment plan will depend on the underlying cause of azoospermia.
One option is surgery. Surgical procedures such as varicocele repairs or transurethral resection may be necessary to treat certain types of azoospermia. Varicocele repair involves repairing the veins that drain the testicles, while transurethral resection involves removing any blockages in the urethra.
Another option is medication. Some medications can help increase sperm production and improve fertility. For example, clomiphene citrate is a medication that stimulates hormones in the brain to increase sperm production.
Therapies such as acupuncture and herbal remedies may also be helpful in treating azoospermia. However, it is important to consult with a healthcare professional before starting any alternative therapies.
Infertility Treatment for Azoospermia
Infertility treatment may involve a combination of treatments, depending on the underlying cause of azoospermia. In some cases, infertility treatments such as intrauterine insemination (IUI) or in vitro fertilization (IVF) may be necessary.
IUI involves placing sperm directly into the uterus during ovulation, while IVF involves fertilizing an egg outside of the body and then transferring it into the uterus. In some cases, donor sperm may also be used for these procedures.
It’s important to note that infertility treatment, including sperm retrieval, can be expensive and not always successful due to low sperm counts. It’s essential to discuss all options with a healthcare professional and thoroughly consider each one before making a decision.
Creating a Treatment Plan for Azoospermia
A treatment plan for azoospermia will depend on an individual’s specific circumstances. A healthcare professional will consider factors such as age, overall health, and the underlying cause of azoospermia.
In some cases, optional therapies or surgical repair may be recommended. For example, testicular sperm extraction (TESE) is a surgical procedure that involves removing sperm directly from the testicles for use in IVF.
It’s important to work closely with a healthcare professional to develop an effective treatment plan for azoospermia. This may involve multiple appointments and tests to determine the best course of action.
Azoospermia Outlook and Prognosis: What to Expect
Azoospermic Men May Have a Poor Prognosis for Natural Conception Due to the Absence of Sperm in Their Semen
Azoospermia is a condition where there is no sperm present in the semen. It can be caused by various factors such as hormonal imbalances, genetic abnormalities, infections, or testicular injury. For men with azoospermia, natural conception may not be possible without medical intervention.
The prognosis for azoospermic men depends on the underlying cause of their condition. If it is due to a genetic abnormality or testicular injury, the chances of successful treatment may be lower than if it is caused by an infection or hormonal imbalance. In some cases, surgical procedures such as micro-TESE (microdissection testicular sperm extraction) may be able to retrieve viable sperm from the testicles that can be used for assisted reproductive technologies (ART) like IVF.
However, even with successful ART treatments, there is still no guarantee of pregnancy. The success rates vary depending on numerous factors such as age of the female partner and quality of retrieved sperm.
Severe Oligozoospermia Can Also Impact Fertility and Require Medical Intervention
Severe oligozoospermia is a condition where there are very few sperm present in the semen. While not as severe as azoospermia, it can still impact fertility and require medical intervention. The prognosis for men with severe oligozoospermia depends on how low their sperm count is and what underlying factors are causing it.
In some cases, lifestyle changes like quitting smoking or reducing alcohol consumption can improve sperm count and quality. Hormone therapy may also help stimulate sperm production in some cases. However, more severe cases may require surgical procedures or ART treatments like ICSI (intracytoplasmic sperm injection) to achieve pregnancy.
Certain Medical Conditions Such as Prostate Cancer and Its Treatments Can Cause Azoospermia or Severe Oligozoospermia, Leading to Potential Fertility Issues
Medical conditions such as prostate cancer and its treatments can cause azoospermia or severe oligozoospermia. Radiation therapy and chemotherapy can damage the testicles and affect sperm production. Surgery to remove the prostate gland may also damage the nerves and blood vessels that are necessary for ejaculation.
For men with prostate cancer who wish to preserve their fertility, options like sperm banking before treatment or surgical procedures like micro-TESE after treatment may be available. However, it is important to discuss these options with a healthcare provider before undergoing any cancer treatments.
While Treatments May Be Effective for Some Men, Failure to Achieve Pregnancy Is Still Possible. These Treatments May Come With Side Effects That Should Be Considered
While treatments like surgery, hormone therapy, and ART may be effective for some men with azoospermia or severe oligozoospermia, failure to achieve pregnancy is still possible. It is important for couples undergoing these treatments to have realistic expectations about their chances of success.
Furthermore, these treatments may come with side effects that should be considered. Hormone therapy can cause mood changes and decreased sex drive in some men. Surgical procedures like micro-TESE for sperm retrieval carry risks of infection and bleeding. ART treatments like IVF can be expensive and emotionally taxing, especially for men with low sperm counts.
It is important for couples considering sperm retrieval and other infertility treatment options to weigh the potential benefits against the risks and costs involved. They should also discuss their options thoroughly with a healthcare provider who specializes in male infertility and can provide guidance on sperm counts.
Importance of Awareness: Deterrence and Patient Education
Azoospermia: An Overview
Azoospermia is a condition that affects men, characterized by the absence of sperm in semen. It is estimated to affect 1% of the male population and can be classified into two types: obstructive and non-obstructive azoospermia. Obstructive azoospermia occurs when there is a blockage or obstruction in the reproductive tract, while non-obstructive azoospermia occurs due to an issue with sperm production.
While some men may not experience any symptoms, others may notice changes such as decreased sex drive, erectile dysfunction, or testicular pain. Additionally, low sperm counts may require sperm retrieval procedures to be performed. As such, patient education about this condition is critical in increasing awareness about its overall incidence rates and ways to manage it.
The Role of Healthy Lifestyle Changes
Patients with azoospermia can benefit from healthy lifestyle changes such as regular exercise and a balanced diet rich in antioxidants. These changes can improve their overall health and potentially reduce the effects of the condition.
Regular exercise has been shown to increase testosterone levels in men which can help improve sperm production. Consuming antioxidant-rich foods such as fruits and vegetables can help reduce oxidative stress which has been linked to infertility issues.
Therapy Options for Azoospermia
Therapy options for azoospermia include sperm retrieval techniques and the use of resistive index to assess testicular function. However, success rates vary depending on the underlying cause of the condition.
Sperm retrieval techniques involve extracting sperm directly from the testes using methods like percutaneous epididymal sperm aspiration (PESA) or testicular sperm extraction (TESE). While these techniques have high success rates for obstructive cases, they may not be effective for non-obstructive cases.
The resistive index is a measure used to assess blood flow within the testicles. It can help determine the presence of any blockages or abnormalities that may be causing azoospermia. However, its effectiveness in predicting fertility outcomes is still being studied.
Underlying Causes of Azoospermia
Data suggests that maturational arrest and the presence of antibodies are common causes of azoospermia. Maturational arrest occurs when sperm production stops at an early stage, while the presence of antibodies can affect sperm function and movement.
Non-obstructive cases with low sperm counts are more resistant to treatment, and it’s essential to identify the underlying cause before deciding on a course of therapy, which may involve sperm retrieval. In some cases, genetic testing may be necessary to determine if there are any chromosomal abnormalities that may be affecting fertility.
The Importance of Seeking Medical Attention
Patient education should also include information about the potential link between azoospermia and testicular cancer, as well as the importance of seeking medical attention if symptoms arise.
Testicular cancer has been linked to infertility issues such as azoospermia. As such, men with this condition should undergo regular screening for testicular cancer to ensure early detection and treatment.
It’s also important for men experiencing symptoms like decreased sex drive or erectile dysfunction, as well as low sperm counts, to seek medical attention promptly. These symptoms could indicate underlying health issues that need immediate attention, which may include sperm retrieval.
Enhancing Healthcare Team Outcomes for Azoospermia Patients
Importance of Comprehensive Care and Support
Male infertility patients with azoospermia require comprehensive care and support from their healthcare team to achieve successful sperm retrieval. The healthcare team, which may include urologists, endocrinologists, and reproductive specialists, plays a crucial role in providing tailored treatment plans that consider the patient’s unique situation.
One important consideration is the use of assisted reproduction techniques such as intracytoplasmic sperm injection (ICSI) to extract viable sperm from infertile men with azoospermia. However, careful evaluation of factors such as sperm quality and erectile dysfunction is necessary before proceeding with this method. The healthcare team should work together to determine the appropriate course of action for each individual patient.
In addition to ICSI, testicular sperm extraction (TESE) is a common method used to extract viable sperm from infertile male patients with azoospermia. This procedure involves removing small amounts of testicular tissue through an incision in the scrotum or lower abdomen. TESE may be combined with exogenous testosterone supplementation or anastrozole to improve fertility outcomes.
Collaborative Efforts Between Healthcare Professionals
Collaborative efforts between healthcare professionals can enhance healthcare team outcomes for azoospermia patients by providing ongoing support for infertile couples. Urologists play a critical role in evaluating and counseling male infertility patients, while endocrinologists can help manage hormonal imbalances that may contribute to infertility.
Reproductive specialists, including those with expertise in sperm retrieval, are also essential members of the healthcare team, providing tailored treatment plans that address the unique needs of each patient through assisted reproduction techniques and fertility treatments. By working together, these professionals can create effective solutions for patients struggling with infertility.
Moreover, it’s important for men with azoospermia to be evaluated and counseled by a specialist as early as possible. Delaying evaluation and treatment can lead to missed opportunities for successful sperm retrieval, which may result in prolonged infertility.
Living with Azoospermia – Coping Strategies and Support
Living with azoospermia can be a challenging experience, but there are strategies and support available to help you cope. Understanding the anatomy of the male reproductive system, exploring the differences between types of azoospermia, understanding underlying factors that cause it, and the tests used in diagnosis can all help in managing this condition.
It’s important to know that you’re not alone in your journey. Statistics show that azoospermia affects many men worldwide. There are also different types of azoospermia, including posttesticular and pretesticular azoospermia. Nonobstructive azoospermia (NOA) is another type that has its own causes and treatment options.
If you’ve been diagnosed with azoospermia, there are management and treatment options available depending on the type of condition you have. These include surgical procedures or fertility treatments like IVF or ICSI.
It’s essential to stay educated about your condition and take advantage of resources available to you such as patient education programs and support groups. Enhancing healthcare team outcomes for azoospermia patients is crucial in providing better care for those affected by this condition.
In conclusion, living with azoospermia can be a challenging experience but being informed about your diagnosis is key to managing this condition effectively. By taking advantage of available resources and support systems, staying positive, and working closely with your healthcare team, you can navigate through this journey successfully.




